Master Services Agreement
Exhibit 10.1

This Master Services Agreement (the “Agreement”) is entered into to be effective as of January 1, 2016 (the “Effective Date”), by and between INOVALON, INC., a Delaware corporation, for its own behalf and on behalf of each of its affiliates (collectively “Inovalon”), and Triple-S Advantage, Inc., administered by Triple- S Advantage Solutions, Inc. (“TSA”) (collectively, “Client”).
Recitals
| A. | Inovalon is a provider of data-driven solutions for the assessment and improvement of clinical and quality outcomes, care management, and financial performance across the healthcare community. Amongst other solution suites, Inovalon provides a suite of technology-enabled solutions designed to enhance Clients’ member disease and co-morbidity identification, encounter facilitation, assessment, data accuracy, documentation, care coordination, decision support, and disease management so as to achieve a broader set of goals inclusive of improving quality of care, clinical outcomes, cost reduction, data accuracy improvement, and clarification of disease and co-morbidity, capitated, and risk-adjusted reimbursement information on behalf of Client. |
| B. | Client is a managed care organization offering one or more Medicare or Medicaid health insurance and/or Part D prescription drug program products under the Medicare Advantage program as described by the Centers for Medicare & Medicaid Services (CMS) and/or Medicaid programs as described by various state health programs in conjunction with CMS. |
| C. | Client wishes to secure the services of Inovalon to provide medical claims data analysis, medical records review, and other services related to the accuracy of Medicare Advantage risk adjustment data upon terms and conditions more fully described in this Agreement and its statements of work. |
| D. | Inovalon and Client are parties to that certain Master Services Agreement effective as of January 1, 2012 which terminates December 31, 2015 and wish to enter into a new agreement as more specifically described herein. |
Agreement
Now, Therefore, in consideration of the mutual covenants and promises contained in this Agreement, and for other good and valuable consideration, the receipt and sufficiency of which is hereby acknowledged, the parties, intending to be legally bound hereby, agree as follows:
1. Services
| 1.1 | Scope of the Services. |
| (a) | Subject to the terms and conditions of this Agreement, Inovalon will perform for Client the services set forth in Statement of Work #1 (Prospective Advantage), Statement of Work #2 (INDICES), Statement of Work #3 (CAAS) and Statement of Work #4 (CARA) (each an “SOW”) attached hereto and incorporated herein (the “Services”). Capitalized terms used but not defined in this Agreement shall have the meanings set forth in the applicable SOW. Additional services may be added from time to time by execution of subsequent statements of work, which services will be thereafter incorporated by reference into this Agreement and will become part of the Services and as well be subject to the terms and conditions of this Agreement. |
Page 2 of 15
| (b) | Client may request any changes to products or services at any time. Each change of product or service will be documented in a change request form and will be signed by both Client and Inovalon. Inovalon will reasonably cooperate with Client’s change requests; will respond to such requests within thirty (30) days with the timeline for the change implementation; and will not unreasonably withhold consent to changes. Additionally, Client may request a change to the composition of the Inovalon team serving Client based on a documented performance or service concern of Client as determined in Client’s sole discretion, including but not limited to the replacement of the account manager assigned by Inovalon, and such request will be accommodated by Inovalon within thirty (30) days of receipt. Also, within sixty (60) days of a request by Client, Inovalon will place an Inovalon employee on site at Client’s office for ongoing service to Client. |
| 1.2 | Performance of the Services. |
| (a) | Inovalon will abide by all applicable federal and state legal requirements with respect to maintaining the confidentiality of Client data received in connection with the Services. |
| (b) | As a business associate of Client, Inovalon will abide by the privacy and security requirements of the Administrative Simplification provisions of the Health Insurance Portability and Accountability Act of 1996, as amended (“HIPAA”), and with the terms and conditions of the Business Associate Agreement attached hereto as Exhibit A. Inovalon will provide its employees and agents and will ensure that its subcontractors receive the necessary training regarding the use and disclosure of PHI pursuant to HIPAA. |
| (c) | In the event Inovalon discovers facts or encounters circumstances materially impairing its ability to perform any of the Services set forth in a SOW, Inovalon will advise Client and Client, at its discretion, may terminate any SOW or the Agreement upon written notice subject to a thirty (30) day cure period (“Cure Period”) as described in Section 3.2(b). If Inovalon has failed to cure the breach within the Cure Period after the receipt of written notice of such breach, Client may give a second notice to Inovalon terminating the applicable SOW or the entire Agreement (excluding any service level or corrective action penalties). Termination of this Agreement will be in addition to and not in lieu of any other rights and remedies available to Client under the Agreement (excluding any service level or corrective action penalties) or at law. A transition process will commence after the second notice of termination is received by Inovalon. Such transition process will include certain activities such as data exchange at no cost. Additional transition requirements will be detailed in each applicable SOW and will include ongoing support from Inovalon until all work is completed, data exchanged, and all tasks performed timely and accurately, according to each SOW. |
| (d) | During the term of this Agreement, Client may review the activities of Inovalon, as they relate to the provision of the Services for Client. Inovalon will cooperate with Client (or its agents as the case may be) in connection with these reviews; provided, however, that (i) Client will give Inovalon reasonable prior notice of such reviews, (ii) Client will conduct each such review in a manner that does not unreasonably interfere with the ongoing activities of Inovalon, and (iii) each party will bear the entirety of its own expenses in association with such reviews. Furthermore, Client reserves the right to review Providers’ and Members’ experience with Inovalon’s provision of Encounter Facilitation and Face-To-Face Member Assessment services. Client may use whichever methods it deems necessary to gather information regarding to Members’ and Providers’ experience with Inovalon, including, but not limited to, the performance of surveys. If Client encounters 50% of negative feedback from Members and/or Providers based on a statistically relevant survey, Client and Inovalon will agree to a corrective action plan as described in Section 9 of this Agreement. |
Page 3 of 15
| (e) | Inovalon will comply with all reporting, file, service, and all other responsibilities as set forth in each SOW. Inovalon will provide Client at least, but not limited to, the reports listed in the Report Inventory attached to this Agreement as Exhibit C. For the sake of clarity, every file and report will be processed and filed within the timelines and completeness standards as defined in the applicable SOW. If Inovalon does not comply with one hundred percent (100%) of such standards for file processing, services, and all other responsibilities, Section 9 will apply. If Inovalon discovers any error or exception within the data delivered or made available to Client within any report, platform, or service, Inovalon will notify Client within twenty four (24) hours and shall take steps to promptly correct such error or exception. Notwithstanding Inovalon’s compliance with this notification and correction requirement, Section 9 will apply. |
| (f) | Inovalon will provide a custom dashboard containing all specific data and reporting as detailed in each SOW. For example, such dashboard shall include, but not be limited to, the following: |
| (i) | Medical Record Review Activities (only to the extent SOW #4 (CARA) remains effective): |
A. The number of targeted CEDI Member Medical Records;
B. The number of digitized medical records;
C. The number of medical records still pending initial review, including the days in aging; and
D. The number of medical records that are completed (completed means submitted through a CMS Risk Adjustment Processing System “RAPS” file and Encounter Data Submission “EDS” file).
| (ii) | ePASS Processing (only to the extent SOW #1 (Prospective Advantage) remains effective): |
A. The number of Member Assessment SOAP Notes completed through ePASS submitted by submission date and submitted through a RAPS File and EDS file;
B. The number of Member Assessment SOAP Notes in ePASS pending to be completed; and
C. The number of Member Assessment SOAP Notes completed through ePASS pending to be reviewed by Inovalon, including the days in aging.
| (iii) | Face-To-Face Member Assessments (only to the extent SOW #1 (Prospective Advantage) remains effective): |
A. The number of Face-To-Face Member Assessments that will be targeted;
B. The number of Face-To-Face Member Assessments already completed at home;
C. The number of Member Assessment Encounter SOAP Notes pending to be reviewed, including the days in aging; and
D. The number of Member Assessment Encounter SOAP Notes that are completed (completed means submitted through a RAPS file and EDS file).
| (iv) | Aggregation activities (only to the extent SOW #3 (CAAS) remains effective): |
A. The number of medical records or health assessment forms supporting codes submitted by Client pending review (coding) including days in aging; and
Page 4 of 15
B. The number of medical records or health assessment forms supporting codes submitted by Client that are completed (completed means through RAPS file and EDS file).
| (v) | For all active SOWs, Inovalon will provide member level report containing number of HCCs targeted and collected by intervention (including source, provider specialty, place of service, and any other agreed upon fields). |
If Inovalon does not comply by having all the data displayed in the custom dashboard as detailed in each SOW, Section 9 will apply. At Client’s request, Inovalon will provide explanations and documentation relating to all data produced by Inovalon in its reports, dashboards, and other services (the “Deliverables”), that are reasonably sufficient for Client to have a clear understanding of the methodology used by Inovalon to generate, and the results, of such Deliverables.
| (g) | In performing services under the Agreement, Inovalon will comply with all requirements set forth in the Medicare Advantage Addendum attached hereto and incorporated into the Agreement as Exhibit B. |
| (h) | The parties will hold a weekly teleconference during the term of the Agreement to discuss Inovalon’s performance under the Agreement and address any issues regarding the Services. When a concern or question relating to the Services is raised in one of these weekly teleconferences by Client, Inovalon will respond to such concern or question within three (3) business days with either (i) a report on the resolution of the issue or answer to the question or (ii) a report acknowledging the issue or question and a timeframe by which Inovalon will resolve the issue or respond to the question. If Inovalon does not comply with subsection 1.2 (h), Section 9 will apply. |
| (i) | If as a result of any error or omission made by Inovalon or any conflict of interest caused by Inovalon in performing Services, CMS or another government agency imposes a penalty on or assesses interest against Client, Inovalon will pay to Client the portion of penalties resulting from Inovalon’s error or omission or from any conflict of interest caused by Inovalon, subject to any limitation of liability described in Section 7.3. This obligation is in addition to any other penalty and indemnification obligations of the parties under this Agreement, and this section shall survive termination of the Agreement or any SOW. Client reserves the right, at its option, to terminate the Agreement for the causes described in this sub-section 1.2(i). Termination of this Agreement will be in addition to and not in lieu of any other rights and remedies available to Client under the Agreement (excluding any service level or corrective action penalties) or at law. |
| (j) | Additional Reporting Requirements. Failure to comply with this Section 1.2(j) may result in penalties as described in Section 9. |
| (i) | Provided Client gives Inovalon an estimate by month of the Member Population by October 1, 2015 for the 2016 calendar year (and by July 1, 2016, for the 2017 calendar year) Inovalon will deliver to Client by November 1, 2015 for the 2016 calendar year (and by August 1, 2016 for the 2017 calendar year) a cost structure worksheet (detailing all estimated activities and associated cost for each calendar year of the Agreement) for Client approval. This worksheet shall be submitted and will be revised as needed during the calendar year and is intended to be used by Client for budget preparation. |
| (ii) | To the extent applicable to the Services, Inovalon will deliver a monthly Risk Adjustment Data Information Attestation to Client attesting that all activities that have been performed and that all data submitted are correct, complete, and truthful to the best of Inovalon’s knowledge. |
Page 5 of 15
| (iii) | Beginning January 2016, Inovalon will provide monthly results of performance on quality metrics from the reviews and audits performed by Inovalon of activities including, but not limited to, the following: |
A. Quality performance insight and reporting;
B. Face-To-Face Member Assessments performed by Inovalon’s subcontracted providers as part of SOW #1 (Prospective Advantage);
C. Outreach percentage of calls performed and completed to members as part of SOW #1 (Prospective Advantage);
D. Telephone numbers from members or providers that are disconnected or incorrect; and
E. For SOW #1 (Prospective Advantage) and SOW #4 (CARA), Inovalon will ensure that the diagnoses provided in the RAPS files will be provided in the EDS files. Inovalon will submit EDS Files in a format that is compliant with CMS’s contractor or Client’s submission system.
| (iv) | Using the reports described in Section 1.2(j)(iii)(A) above, Inovalon will incorporate into its medical record reviews process and internal training a coding quality analysis with the goal of improving coding accuracy. |
| (k) | Audits. Client reserves the right to audit Inovalon’s compliance with the Agreement at any time while the Agreement is in effect, and for one year after the Termination Date (except that there shall be no time limit on audits either related to or initiated by a government agency audit request or investigation or in connection with a lawsuit or audit initiated by Client triggered by a government audit. These audits will include, but are not limited to, the Risk Adjustment Data Validation (RADV) process. In connection with audits under this Agreement, Inovalon will make available records and information of its subcontractors (or Downstream Entities as defined in Exhibit B) related to the services provided under this Agreement, as described in more detail in Section 3.1 of Exhibit B (Medicare Addendum). Client will provide Inovalon with reasonable prior notice of such audit (if the audit is initiated by Client and not a regulatory entity) or once Client is notified of an audit by federal or local regulators. Inovalon shall cooperate with any form of audit, internal or external, including those performed by CMS or another government agency or by Client and/or its agents, as the case may be. If as a result of a finding regarding Inovalon’s Services performed on behalf of Client, CMS or another government agency imposes a penalty on or any other fine or assessment (including but not limited to interest) against Client, Inovalon will reimburse Client in accordance with Section 1.2(i) of this Agreement. In case of a finding by Client, CMS or another government agency, Inovalon shall submit a corrective action plan within the required timeframes established. The Corrective Action Plan will contain information including, but not limited to: Root Cause analysis, Activities to correct the finding to avoid recurrence, responsible person, due date monitoring activities and training, among others. The remedies set forth in this Section 1.2 (k) of the Agreement shall be in addition to and not in lieu of any other rights and remedies available to Client under the Agreement (excluding any service level or corrective action penalties) or at law. In addition, upon request by Client, Inovalon will provide its annual Statement on Standards for Attestation Engagements (SSAE No. 16) SOC 1 Type 2 (or equivalent) audit reports to Client. Such report will be considered confidential and proprietary to Inovalon. |
| (l) | RAPS and EDS Files. Inovalon shall prepare and process RAPS files under each SOW in accordance with CMS regulations and instructions. RAPS files must be complete and accurate based on the information provided to or collected by Inovalon and submitted to Client timely, at least monthly or as mutually agreed upon by Client and Inovalon. During the period beginning four (4) weeks prior to the due date for RAPS files under SOW #4 (CARA) to be submitted to CMS (the “Sweep Period”), RAPS will be submitted at weekly intervals if reasonably requested by Client to enable Client to submit its files before the end of the Sweep Period. For SOW #1 (Prospective Advantage) and SOW #4 (CARA), every RAPS file shall be accompanied by an EDS file (except for claims RAPS). |
Page 6 of 15
| 1.3 | Client Responsibilities. To assist Inovalon in the performance of its responsibilities under this Agreement, Client agrees to perform the following duties: |
| (a) | To provide for those Client responsibilities set forth on the statements of work attached hereto or as may be added by amendment to this Agreement. |
| (b) | To provide Inovalon with all information reasonably required for the provision of the Services. |
| (c) | To notify Inovalon, in writing, with regard to any operational matter not acceptable to Client. Inovalon will acknowledge in writing to Client its receipt of such written notice within seven business days following such receipt. Inovalon will thereafter, but in no event later than 14 days after its receipt of such written notice, take every reasonable action necessary to correct such matter and if not, it shall be considered a material breach subject to termination by Client as provided in Section 3.2(b) of this Agreement. |
2. Inovalon Status; Client Decisions
| 2.1 | Independent Contractor Status. Inovalon is an independent contractor performing certain project management, data processing and analysis services for Client and is not an employee, agent, representative, officer, or partner of Client. Except as expressly set forth in this Agreement, Inovalon has no power or authority to act for, represent, or bind Client in any manner. Nothing contained in this Agreement will be deemed to create any relationship between the parties other than that of a principal and independent contractor. |
| 2.2 | Inovalon Services and Client Decisions. The parties acknowledge the importance of risk adjustment related data that is submitted to CMS for the purpose of calculating reimbursement by the federal government to Client for its Medicare Advantage plans, as well as the legal risk associated with any submissions by Client of inaccurate or unsubstantiated diagnosis codes for members. Inovalon agrees to provide Client with accurate and substantiated diagnosis-related information and other data that can be relied upon by Client to make decisions about what information may be submitted to CMS for the purpose of reimbursement under Client’s Medicare Advantage plans. |
3. Term and Termination
| 3.1 | Term. This Agreement and the SOWs will remain in effect until December 31, 2017, the “Termination Date.” A transition process shall begin sixty (60) days prior the Termination Date, which will include the items specifically called out in each applicable SOW. All services being performed under one or more SOWs will be completed within ninety (90) days following the Termination Date, all as more specifically set forth in the applicable SOW. Such transition process will include ongoing support from Inovalon until all interventions scheduled prior to the Termination Date are performed, data exchanged, and all tasks relating to Inovalon’s Services are performed timely and accurately, according to CMS and Puerto Rico Health Insurance Administration (ASES by its Spanish acronym) regulations. Upon termination of the Agreement, the parties agree that Inovalon will provide the transition services described in this Section 3, as outlined within the Cost of Transition Period applicable to each SOW. |
| 3.2 | Termination. This Agreement will terminate upon occurrence of any of the following events: |
Page 7 of 15
| (a) | Upon written notice to Client for any failure to make payments to Inovalon when due, which failure remains uncured for a period of thirty (30) days after receipt by Client of written notice of such breach; |
| (b) | Upon written notice to the breaching party for a material breach of the Agreement (other than for failure to pay), which breach remains uncured for a period of thirty (30) days after receipt of written notice specifying the breach; or |
| (c) | Either party is adjudged bankrupt, makes a general assignment for the benefit of creditors, seeks reorganization under bankruptcy or insolvency laws, or a proceeding relating to bankruptcy or insolvency laws is commenced against the other party. |
| (d) | In the event of a termination of this Agreement for breach of this Agreement by Client, notwithstanding anything herein to the contrary, Client will be responsible for all of the fees which would have otherwise been due under this Agreement for the remainder of the term if not for such breach. |
| (e) | In no event shall this Agreement survive upon termination of the Services set forth in Statement of Work #1 (Prospective Advantage), Statement of Work #2 (INDICES), Statement of Work #3 (CAAS) and Statement of Work #4 (CARA), as well as any other additional services which may be later added by execution of subsequent statements of work incorporated by reference into this Agreement. |
| 3.3 | Survival. Notwithstanding anything to the contrary contained in this Agreement, the provisions of Sections four (4), five (5), six (6), seven (7), eight (8) and Exhibit A will survive any termination, expiration or cancellation of this Agreement, regardless of the basis for such termination or cancellation. |
4. Payments
| 4.1 | Fees. Client will pay Inovalon for the Services in accordance with the reimbursement and payment schedules set forth in any SOW attached hereto and except as specified in any SOW, Inovalon will invoice Client for the Services provided on a monthly basis in arrears. Invoices will be entirely accurate, state all charges broken down by each SOW, and specify the measurement unit for each category of service. In case of any increments in cost, each additional increment will also be broken down by category and unit. Individual invoices will be made for each SOW, and Inovalon will provide a monthly attestation as to the accuracy of invoices submitted, in a form satisfactory to Client. |
| 4.2 | Payment Term. Payment to Inovalon is due thirty (30) days from the date of receipt of the undisputed invoice by Client provided, however, that this thirty (30) day period shall not begin to run unless and until Client receives an invoice that meets all of the requirements set forth in Section 4.1 above. |
| 4.3 | Late Charges. If any undisputed fee for services by Inovalon is not paid by the due date thereof, interest will accrue from such due date at a rate equal to one point five percent (1.5%) per month. Client will pay such interest upon demand by Inovalon that will be in addition to the amounts charged by Inovalon for its services. The amount of interest payable pursuant to this provision will not exceed the maximum effective rate of interest permitted to be paid under applicable law. If such amounts result in an effective rate of interest in excess of the maximum as permitted under applicable law, then the amount payable pursuant to this provision will be reduced to the highest amount permitted under such applicable law. |
| 4.4 | Annual Adjustments. Each of the fees outlined within any SOW will be subject to adjustment on an annual basis with the first adjustment occurring on January 1, 2017 (the “Annual Adjustment”) which will be equal to 1.5% over the previous annual period of this Agreement. As soon as practicable following each anniversary of the effective date of the applicable SOW, Inovalon will notify Client in writing of the occurrence and amount of any Annual Adjustment, which will be reflected in invoices issued thereafter. |
Page 8 of 15
| 4.5 | Additional Payment Terms. |
| (a) | Identified credits due to Client, including but not limited to credits due as a result of penalties imposed under this Agreement, will be applied by Inovalon in the next month’s invoice for which the credit applies. If credits cannot be applied to future fees because the Agreement has terminated, Inovalon will pay Client the amount of the credit. |
| (b) | Inovalon will make available supporting reports for invoices to enable Client to audit and verify charges for Services performed. |
| (c) | Client will reimburse Inovalon for travel expenses incurred in performing Services only if such expenses are directly attributable to the Services performed for or provided to Client. Inovalon will provide appropriate vouching documentation for all expenses. Client will reimburse Inovalon for any expense that Client has pre-approved in writing. Notwithstanding the foregoing, Client will not pay any expenses incurred or caused by any error or omission of Inovalon, or any of its officers, directors, employees and agents. |
| (d) | Inovalon will provide support services in addition to the Services described in this Agreement and the SOWs to Client at the rates described in each SOW. |
5. Proprietary Information; Rights, Use, and Ownership
| 5.1 | Definition. The parties acknowledge that both parties may own, utilize, and develop certain Proprietary Information (as defined herein) during the course of the Agreement and in furtherance of their respective obligations thereunder, which is privileged and confidential. “Proprietary Information” includes trade secrets and computer programs and software (including source codes), processes, technical information, know-how, plans, specifications, identity of customers and suppliers, financial information, and other proprietary or confidential information related to the Services and business affairs of the party which is treated as confidential by such party; provided, however, that Proprietary Information will not include information which is known or becomes known to the public in general (other than by a breach of this provision), is or has been independently developed or conceived by the other party without the use of the first party’s Proprietary Information, or is or has been made known or disclosed to the other party by a third person without a breach of any obligation of confidentiality such third person may have to the first party. All such information shall be deemed Proprietary Information whether or not identified as such prior to or at the time of disclosure. |
| 5.2 | Use, Disclosure. The parties agree that both parties will disclose Proprietary Information to the other party only to the extent that such information is necessary to conduct the Services. With respect to any Proprietary Information disclosed by a party (the “Disclosing Party”) to the other party (the “Receiving Party”) the Receiving Party will not report, publish, transfer or otherwise disclose such information to any person, company or other entity (except that such disclosure may be provided to an affiliated or contracted or subcontracted entity or person who is bound by formal contract, including confidentiality provisions of materially similar nature, with Receiving Party) without the prior written consent of the Disclosing Party or except as otherwise expressly permitted by the terms of this Agreement, and the Proprietary Information will not be utilized for the detriment or intended detriment of the Disclosing Party, including the solicitation of any of that party’s customers, members or employees. If any court or government agency requires either party to disclose Proprietary Information covered by this Agreement, then the required party may make any disclosure required by law. In such situation the required party will provide other party with prompt notice of any such requirement prior to disclosure of the information and consult them, whenever possible in responding to it. Upon request of the Disclosing Party after expiration or earlier termination of this Agreement, unless otherwise stated in this Agreement the Receiving Party shall immediately cease using and within thirty (30) days following request shall promptly redeliver to the Disclosing Party all Proprietary Information and any other material containing or reflecting any Proprietary Information, including but not limited to all tangible materials, as well as all machine-readable media which in any way relate to the Proprietary Information. Receiving Party agrees not to retain any copies, extracts or other reproductions in whole or in part of the above materials, whether tangible or stored in any computer memory or storage medium; or if the Disclosing Party directs in writing, destroy all Proprietary Information disclosed in or reduced to tangible form including all documents, memoranda, notes, summaries, compilations, analyses, notes and other writings whatsoever, and any copies thereof, prepared by the Recipient or its Representatives based on, or derived from the Proprietary Information, and such destruction shall be certified in writing to the Disclosing Party by an authorized officer supervising such description. If it is necessary for any legal or regulatory requirement, Recipient is allowed, previous notification to Disclosing Party, to maintain one copy of the above mentioned documents. The parties acknowledge that no license is created by the use of the Proprietary Information beyond that which is contemplated within the scope of this Agreement. It is further acknowledged and understood that Inovalon may use de-identified data and other Inovalon Intellectual Property, independently and in aggregation with other healthcare data, to perform analysis, including disease trends, statistical and internal system analytics, and such other analytics as Inovalon may perform from time to time for the improvement of healthcare and industry-related insights, as well as additional analytics related to assessment of the member population and opportunities to improve the payment, treatment and healthcare operations of Client. |
Master Services Agreement
Page 9 of 15
| 5.3 | Client Right to Use Inovalon Intellectual Property. Inovalon hereby grants to Client a royalty-free, perpetual license and the right to use, copy, and maintain Inovalon Intellectual Property (defined below) and data that has been fully paid for by Client and provided to or collected by Inovalon for Client for the purposes of Client’s: (a) CMS reporting, regulatory, and quality management; (b) internal or external evaluations; and (c) other purposes that do not violate the provisions of this Agreement. |
| 5.4 | Ownership of Intellectual Property. Inovalon is the sole owner of all Inovalon -created deliverables; data collection, processing, analysis, review, and reporting tools; data processing and management systems or processes, including all tangible and intangible items, the MORE2 Registry, processes, or information collected, clarified, processed, or incorporated therein or thereby; and all copyrights and other intellectual property rights pertaining thereto (collectively, the “Inovalon Intellectual Property”). Moreover, it is understood that data may be utilized by Inovalon to influence and inform its Services and enhance analytical insights, which become part of the Inovalon Intellectual Property. Without limiting the generality of the foregoing, it is expressly acknowledged that Inovalon Intellectual Property includes the marks “CARA”, “CAAS”, “ChaseWise”, “CCS Advantage”, “CareSync Advantage”, “CQM”, “EMR Acceleration”, “ePASS”, “HEDIS Advantage”, “iDCT”, “INDICES”, “Insights”, “MORE² Registry”, “PCIS”, “Prospective Advantage”, “QSFD”, “QSI”, “Quality Spectrum Hybrid Reporter”, “Star Advantage”, and all other trade, service, and other marks of Inovalon, all rights to which are held by Inovalon and expressly retained thereto. If any such Inovalon -created deliverables or other Inovalon Intellectual Property may, by operation of law, be considered “works made for hire” (or if ownership of all right, title and interest of copyrights therein will not otherwise vest exclusively in Inovalon), then Client will be deemed to have hereby automatically assigned, without further consideration, the ownership of all copyrights therein to Inovalon, its successors and assigns. Inovalon, its successors, and assigns will have the right to obtain and hold in its or their own name copyrights, registrations and any other protection available in the foregoing. Client agrees that it will not market, parcel, distribute, sell or otherwise communicate the Inovalon Intellectual Property without the express written consent of Inovalon. Moreover, it is acknowledged and understood that Inovalon will have a royalty-free, perpetual license to use or incorporate into the Inovalon Intellectual Property any suggestions, enhancements requests, recommendations or other feedback provided by Client. Notwithstanding anything herein to the contrary, to the extent Client engages Inovalon to perform custom work and deliverables, the parties will detail such custom work and deliverables in writing and such custom work and deliverables will be considered “works made for hire.” |
Master Services Agreement
Page 10 of 15
| 5.5 | Equitable Relief. Since a remedy at law for any breach or attempted breach of the provisions of this Section 5 will be inadequate, either party hereto will be entitled to specific performance and injunctive or other equitable relief, without bond, in case of any such breach or attempted breach, in addition to any remedies available at law. No remedy conferred on Disclosing Party by any of the specific provisions of this Section 5.5 is intended to be exclusive of any other remedy, and each and every remedy shall be cumulative and shall be in addition to every other remedy given or now or later existing at law or in equity or by statute or otherwise. The election of one or more remedies by the Disclosing Party shall not constitute a waiver of the right to pursue other available remedies. If legal action is required for the enforcement of the terms of this Section 5, the prevailing party shall be entitled to recover any and all of its costs and expenses, including without limitation reasonable attorney’s fees. |
6. Resolution of Disputes
| 6.1 | Duty to Negotiate in Good Faith. If a party has reason to believe the existence of a dispute in connection with this Agreement and the Services provided hereunder, it will give written notice to the other party, describing the dispute and a proposed resolution. The parties will then meet as soon as practicable thereafter and negotiate in good faith to resolve the dispute. |
| 6.2 | Arbitration. If the dispute cannot be resolved by way of direct negotiation within thirty (30) days of notice of a dispute having been given as described above, the dispute will be decided by arbitration upon initiation by either party, which will be conducted by a single arbitrator and, except as otherwise expressly provided herein, in accordance with the complex commercial dispute rules of the American Arbitration Association, unless the parties mutually agree that another arbitration provider and its binding arbitration rules will be used in this case. The arbitration will be conducted in Miami, Florida unless the disputing parties mutually agree otherwise. In the event that there will be more than one dispute to be arbitrated, the parties agree that all pending disputes will be consolidated to the extent feasible. Within thirty (30) days of the hearing, the arbitrator will render a decision concerning all contested issues considered during the arbitration and the arbitrator will notify the parties in writing of his or her decision, setting forth the arbitrator’s findings of fact and conclusions of law and the dollar amount, if any, awarded. Unless the parties mutually agree otherwise, the arbitrator may fix his or her compensation. The fees of the American Arbitration Association (or other agreed upon provider) and of the arbitrator will be paid equally by the parties, unless the arbitrator determines that a particular party has prevailed on all major substantive issues presented, in which case the fees and costs will be paid by the party not so prevailing. This agreement to arbitrate will be specifically enforceable under the Florida Arbitration Act. The arbitrator’s decision will be final, and judgment, including specific enforcement of the decision, may be entered upon the decision in any court of competent jurisdiction in accordance with applicable law. The amount of any dollar award, including applicable fees and costs of the prevailing party, will be paid in cash by the party not so prevailing to the prevailing party, within thirty (30) days following the date of such award. In the event that payment is not made within the time period provided herein, the prevailing party will have the right to commence an action, at law or in equity, in any state or federal court in the State of Florida to have the decision of the arbitrator enforced. In the event such an action is filed, the costs of such action (including in-house counsel fees) will be borne by the party against whom such performance is sought. A pending arbitration will not extend the term of this Agreement or affect any termination provided for hereunder. All statutes of limitations will be tolled from the date of giving notice of the intention to submit to arbitration and for ninety (90) days after the delivery of the arbitrator’s written determination. |
| 6.3 | Equitable Relief. To the extent that the arbitrator acting under the applicable rules of the American Arbitration Association (or other agreed upon provider) and pursuant to Florida law does not have legal jurisdiction and authority to impose injunctive or other equitable relief, a party seeking the same will be entitled to pursue the same through court litigation. Such action may be pursued during, after or in lieu of arbitration. Any such action will be pursued only in the state or federal courts with requisite jurisdiction located in Miami, Florida. |
Master Services Agreement
Page 11 of 15
7. Indemnification; Limitation of Liability; Disclaimer; Insurance
| 7.1 | Indemnification of Inovalon. Client will indemnify and hold Inovalon and its officers, directors, employees, agents, consultants, affiliates, and representatives harmless from and against any and all actions, suits, proceedings, liabilities, losses, damages, judgments, fines, amounts paid in settlement, losses, costs and expenses which may arise out of acts or omissions of Client or its officers, directors, employees, agents, consultants, affiliates, and representatives in the performance of Client’s responsibilities under this Agreement or which may arise out of any action or decision taken, made, or authorized by Client. Additionally, Client will indemnify Inovalon to the extent Inovalon acts specifically at the direction of Client. |
| 7.2 | Indemnification of Client. Inovalon will indemnify and hold Client and its officers, directors, employees, agents, consultants, affiliates, and representatives harmless from and against any and all actions, suits, proceedings, liabilities, losses, damages, judgments, fines, amounts paid in settlement, losses, costs and expenses which may arise out of acts or omissions of Inovalon or its officers, directors, employees, agents, consultants, affiliates, and representatives in the performance of its or their responsibilities under this Agreement. |
| 7.3 | Limitations of Liability. Except for any intentional infringement of a party’s proprietary rights as provided in Section 5, in no event will either party hereto be liable to the other party under this Agreement or otherwise for any special, consequential, punitive, exemplary, reliance, indirect or incidental damages, whether under theories of contract, tort, or otherwise, even if such damages were foreseeable. In addition, in no event will either party’s liability arising out of or related to this Agreement exceed the sum of fees paid by Client for the SOW giving rise to the liability during the one-year period immediately preceding the date the cause of action arose. Notwithstanding the foregoing limitation, for (i) government fines due solely to a party’s acts or omissions or (ii) liability resulting from False Claims Act litigation, in no event will either party’s liability arising out of or related to this Agreement exceed the greater of (A) Ten Million Dollars ($10,000,000) or (B) the sum of fees paid by Client for the SOW giving rise to the liability during the one-year period immediately preceding the date the cause of action arose. |
| 7.4 | Disclaimer. To the extent Inovalon develops measures for Client, the development of such measures and related materials regarding Client in no way constitutes a warranty by Inovalon to Client, Client’s enrollees or any other third parties with respect to the quality or nature of health services provided to enrollees. Furthermore, Client acknowledges that Inovalon shall not be liable for any disclosure or dissemination of measures. Except as expressly provided herein, Inovalon makes no warranties of any kind, whether express, implied, statutory, or otherwise and specifically disclaims all implied warranties, including any warranties of merchantability or fitness for a particular purpose, to the maximum extent permitted by applicable law. |
| 7.5 | Insurance. Inovalon shall procure and maintain at its own expense, in full force and effect at all times, (including without limitation, the timely payment of all premiums), during which the Services are rendered under this Agreement: (a) Professional Liability coverage with limits in the amount of $1,000,000 per occurrence and $3,000,000 in the aggregate; (b) Workers Compensation and Employer’s Liability Insurance with the minimum limits of $1,000,000; and (c) Comprehensive General Liability insurance with combined single limit for bodily injury and property damage in the amount of $2,000,000. Inovalon will provide to Client a certificate of insurance each year upon Client’s request. |
8. Miscellaneous
| 8.1 | Notices. All notices, consents, waivers and other communications under this Agreement must be in writing and will be deemed to have been duly given when (a) delivered by hand (with written confirmation of receipt), (b) sent by facsimile or electronic mail (with written confirmation of receipt), provided that a copy is mailed by registered mail, return receipt requested, or (c) when received by the addressee, if sent by a nationally recognized overnight delivery service (receipt requested), in each case to the appropriate addresses and facsimile numbers set forth on the signature page below (or to such other addresses and facsimile numbers as a party may designate by notice to the other party). |
Master Services Agreement
Page 12 of 15
| 8.2 | Mutual Agreement Not to Solicit Employees. During the term of this Agreement and for a period of one year thereafter, neither party will, either directly or indirectly, on its own behalf or on behalf of others, solicit, divert or hire away, or attempt to solicit, divert, or hire away, any person employed by the other party, whether or not such employee is a full-time employee or a temporary employee of, consultant to, or independent contractor to such other party and whether or not such employment or engagement is pursuant to written agreement and whether or not such employment or engagement is for a determined period or is at will. Notwithstanding the foregoing, this provision is not intended to preclude a party from hiring persons responding to a general solicitation, provided such party does not knowingly violate the provisions of this Section 8.2 or conduct such general solicitation in a manner intended to circumvent the terms thereof. |
| 8.3 | Entire Agreement and Modification. Except as described in this Section 8.3, this Agreement, together with all referenced and attached exhibits, contains the entire agreement between the parties hereto, supersedes all prior agreements, arrangements, or understandings between the parties and constitutes a complete and exclusive statement of the terms of the agreement between the parties with respect to its subject matter. This Agreement may not be modified or amended except by a written agreement duly signed by persons authorized to act on behalf of the party to be charged with the amendment. |
| (a) | 2012 Agreement. It is understood that this Agreement is replacing the Master Services Agreement effective as of January 1, 2012 (the “2012 Agreement”). The 2012 Agreement will become null and void upon the Effective Date and neither party will have any further rights or obligations to the other under the 2012 Agreement. Notwithstanding the foregoing, any CARA Processes in process as of the Effective Date (namely, the 2015 RRO Process) will be governed by the terms and conditions of Statement of Work #5 to the 2012 Agreement. For the sake of clarity, the RRO Process for the 2015 calendar year RRO Process DOS Period will be performed and invoiced as described in Statement of Work #5 to the 2012 Agreement. |
| 8.4 | Limited Consent. The parties mutually agree to allow the other the use of its name and associated marks for purposes of client references and otherwise identifying the presence of the relationship and both parties acknowledges that they have no ownership right or interest in the trademarks or trade names of the other party. In the setting of a party desiring or otherwise needing to make a public announcement, both parties agree to cooperate in good faith and will have the right to review the relevant portions of such announcement containing reference to its name or marks, and use of the other party's name and/or marks will be allowed with the consent of such party, which consent will not be unreasonably withheld or delayed. Inovalon recognizes and agrees that no public use of Client’s trademarks and trade names may be made without Client’s prior approval not to be unreasonably withheld or delayed and will cooperate with Client in order to comply with Client’s requirements and rules with respect to the co-branding of any materials and use of trademarks and trade names. |
| (a) | Since a remedy at law for any breach or attempted breach of the provisions of this Section 8.4 will be inadequate, either party hereto will be entitled to specific performance and injunctive or other equitable relief, without bond, in case of any such breach or attempted breach, in addition to any remedies available at law. No remedy conferred on the Client by any of the specific provisions of this Section is intended to be exclusive of any other remedy, and each and every remedy shall be cumulative and shall be in addition to every other remedy given or now or later existing at law or in equity or by statute or otherwise. The election of one or more remedies by the Client shall not constitute a waiver of the right to pursue other available remedies. If legal action is required for the enforcement of the terms of this Section, the prevailing party shall be entitled to recover any and all of its costs and expenses, including without limitation reasonable attorney’s fees. |
Master Services Agreement
Page 13 of 15
| 8.5 | Assignments, Successors and Third-Party Rights. Neither party may assign any of its rights under this Agreement without prior written consent of the other party; provided, however, such consent will not be necessary in connection with an assignment on the part of either party of this Agreement to (a) an affiliate of such party as a part of any reorganization or corporate restructuring including a merger or similar transaction, or (b) a third party upon the acquisition by such third party of materially all of the business and assets of the respective party. Subject to the preceding sentence, this Agreement will apply to, be binding in all respect upon and inure to the benefit of the respective successors and permitted assigns of the parties. Nothing expressed or referred to in this Agreement will be construed to give any person other than the parties to this Agreement any legal or equitable right, remedy or claim under or with respect to this Agreement or any provision of this Agreement. This Agreement and all of its provisions and conditions are for the sole and exclusive benefit of the parties to this Agreement and their successors and permitted assigns. |
| 8.6 | Force Majeure; Limitations of Data Accuracy. Neither party will be liable to the other or be deemed to be in breach of this Agreement for any failure or delay in rendering performance arising out of causes beyond its reasonable control and without its fault or negligence. Such causes may include acts of God or of a public enemy, acts of terrorism, earthquakes, floods, fires, epidemics, riots, quarantine restrictions, strikes, freight embargoes, or unusually severe weather. Dates or times of performance will be extended to the extent of delays excused by this section. The parties will promptly inform and consult with each other as to the existence and nature of such delay. Moreover, both parties acknowledge that the accuracy and completeness of the Services may be limited by inaccuracies and incompleteness, if any, within data provided by Client to Inovalon. |
| 8.7 | Maintenance of Copies / Duplicate Records. Notwithstanding anything herein to the contrary, if Inovalon has delivered to Client a complete copy of all MRR Data Sets, all resulting RAPS Files and EDS files, and all reports provided by Inovalon in the provision of the Services, Inovalon may destroy any copies of any or all data, associated reports, or records maintained by Inovalon in association with Client or the services provided to Client and Inovalon will be under no further obligation to maintain any copies of data or records that duplicate the data and records provided to Client hereunder. |
| 8.8 | Severability. If any provision of this Agreement is held invalid or unenforceable by any court of competent jurisdiction or an arbitrator pursuant to Section 6.3 hereof, the other provisions of this Agreement will remain in full force and effect. Any provision of this Agreement held invalid or unenforceable only in part or degree will remain in full force and effect to the extent not held invalid or unenforceable. |
| 8.9 | Section Headings, Construction. The headings of sections in this Agreement are provided for convenience only and will not affect its construction or interpretation. All words used in this Agreement will be construed to be of such gender or number as the circumstances require. Unless otherwise expressly provided, the word “including” does not limit the words or terms preceding it. |
| 8.10 | Governing Law. This Agreement will be governed by and interpreted pursuant to the laws of the State of Florida without regard to conflicts of laws principles. |
| 8.11 | Counterparts. This Agreement may be executed in one or more counterparts, each of which will be deemed to be an original copy of this Agreement and all of which, when taken together, will be deemed to constitute one and the same instrument, and will become effective when there exist copies hereof (by facsimile or otherwise) which, when taken together, bear the authorized signatures of each of the parties. |
| 8.12 | Subcontractors. Except for in connection with the subcontracting of various administrative / back-office processes inherent in the day-to-day operations of Inovalon, Inovalon shall obtain written approval from Client before engaging with any outside firm, through subcontracts or otherwise, to provide any of the services contracted herein. No later than five (5) business days following execution of this Agreement (for calendar year 2016) and September 1 2016 (for calendar year 2017), Inovalon will submit a list of proposed subcontractors for the following calendar year for Client’s review and approval. Client will review the proposed subcontractors to confirm that they are satisfactory to Client, including but not limited to that the subcontractors are not providers in Client’s Medicare Advantage network, and will respond to Inovalon with Client’s approval or disapproval fifteen (15) business days. If Inovalon proposes to add a subcontractor off-cycle, Inovalon will bring such subcontractor to Client for review and approval in Client’s sole discretion. Inovalon will require its approved subcontractors of Services to use contractors for Face-to-Face Member Assessments who are not network providers of Client and do not have a provider services agreement with Client to provide healthcare services under Client’s Medicare Advantage products. |
Master Services Agreement
Page 14 of 15
| 8.13 | No Waiver. The failure of either party at any time to enforce any right or remedy available to it under this Agreement with respect to any breach or failure by the other party shall not be construed to be a waiver of such right or remedy with respect to any other breach or failure. |
9. Corrective Action Plans, Penalties, Service Level Agreements.
| 9.1 | In the event that Client notifies Inovalon of a failure by Inovalon to perform the Services or a material deficiency on the part of Inovalon is discovered pursuant to an audit as permitted by Section 1.2(d) of the Agreement (and such failure or deficiency is solely due to the actions or lack of actions of Inovalon), Inovalon agrees to develop and submit a Corrective Action Plan (CAP) to be reviewed and approved by Client. Client will propose a penalty for Inovalon’s failure to meet the requirements of the CAP. The CAP will establish a timeline for correcting any deficiencies and will include the penalty for Inovalon’s failure to meet the requirements of the CAP in accordance with the timelines therein. If Inovalon fails to comply with the requirement of the CAP by the final completion date of such CAP as designated therein (the “CAP Completion Deadline”), it will be considered a material breach of the SOW for which the CAP was addressed subject to termination in accordance with Section 3.2(b) of the Agreement. |
[SIGNATURE PAGE FOLLOWS]
Master Services Agreement
Page 15 of 15
Intending to be Bound, the parties have caused this Agreement to be executed and delivered by their duly authorized officers or agents as set forth below.
|
|
INOVALON, INC.
|
||
|
|
“Inovalon”
|
||
|
|
|
|
|
| By: | /s/ Xxxxx Xxxxxxxx | ||
| Name: |
Xxxxx Xxxxxxxx, M.D.
|
||
| Title: | CEO | ||
|
Address:
|
|||
|
0000 Xxxxxxxxxx Xxxx
|
|||
|
Xxxxx, Xxxxxxxx 00000
|
|||
|
Tel: (000) 000-0000
|
|||
|
Fax: (000) 000-0000
|
|||
|
Email: xxxxx@xxxxxxxx.xxx
|
|||
|
TRIPLE-S ADVANTAGE INC.
|
|||
|
“Client”
|
|||
| By: |
/s/ Xxxxxxxx Xxxxxxxxx Xxxxxxx
|
||
| Name: |
Xxxxxxxx Xxxxxxxxx Xxxxxxx
|
||
| Title: |
President & CEO
|
||
|
Address:
|
|||
|
XX Xxx 00000
|
|||
|
Xxx Xxxx, XX 00000
|
|||
|
Attn: Xxxxxx Xxxxx
|
|||
|
Tel: 000-000-0000
|
|||
| Email:xxxxxx@xxxxxxxxxxxx.xxx | |||
Master Services Agreement
Exhibit A – Business Associate Agreement
EXHIBIT A
BUSINESS ASSOCIATE AGREEMENT
REGARDING THE USE AND DISCLOSURE OF PROTECTED HEALTH INFORMATION
This Agreement is entered into effective as of January 1, 2016 by Triple-S Advantage, Inc., (heretofore, the Covered Entity) a corporation duly organized under the laws of the Commonwealth of Puerto Rico, and Inovalon, Inc. (heretofore, the Business Associate). This document amends and is part of the Agreement already executed between the PARTIES.
WHEREAS, the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) and its implementing regulations (45 Code of Federal Regulations Parts 160 and 164) impose on Covered Entity and its Business Associates rules relating to the security, use, storage, transmission, and disclosure of protected health information pertaining to participants and beneficiaries of health plans in order to protect and adequately manage protected health information; and
WHEREAS, Business Associate will be granted access to Protected Health Information of Covered Entity to perform its obligations under the underlying Agreement.
NOW, THEREFORE, in consideration of the mutual promises and covenants contained herein and other good and valuable consideration, intending to be legally bound hereby, Covered Entity and Business Associate hereby agree as follows:
Section 1. Definitions
“Business Associate” shall mean Inovalon, Inc. A Business Associate, with respect to a covered entity, is a person or entity who:
(i) On behalf of such covered entity, but other than in the capacity of a member of the workforce of such covered entity or arrangement, performs, or assists in the performance of:
| (A) | A function or activity involving the use or disclosure of individually identifiable health information, including claims processing or administration, data analysis, processing or administration, utilization review, quality assurance, billing, benefit management, practice management, and repricing; or |
| (B) | Any other function or activity regulated by this subchapter; or |
(ii) Provides, other than in the capacity of a member of the workforce of such covered entity, legal, actuarial, accounting, consulting, data aggregation (as defined in 45 CFR § 164.501), management, administrative, accreditation, or financial services to or for such covered entity, where the provision of the service involves the disclosure of individually identifiable health information from such covered entity or from another business associate of such covered entity or arrangement, to the person or entity.
“Covered Entity” shall mean Triple-S Advantage, Inc. A covered entity may be:
(i) A health plan.
(ii) A health care clearinghouse.
Master Services Agreement
Exhibit A – Business Associate Agreement
(iii) A health care provider who transmits any health information in electronic form in connection with a transaction covered by this subchapter.
“Designated Record Set” shall mean the enrollment, payment, claims adjudication and case management record systems maintained by or for a health plan or used in whole or in part, by or for the plan to make decisions about individuals.
“Disclosure” shall mean the release, transfer, provision of access to or divulgation in any manner of information outside the entity holding the information.
“Effective date” shall mean the day and year first above written. “Individual” shall mean the person who is the subject of Protected Health
Information and shall include a person who qualifies as a personal representative in accordance with 45 CFR 164.502(g).
“Privacy Rules” shall mean the Standards for Privacy of Individually Identifiable Health Information as set forth under 45 CFR Part 160 and Part 164, Subparts A and E, as amended.
“Protected Health Information (PHI)” shall mean any information, whether oral or recorded in any form or medium that: (1) is created or received by a health care provider, health plan, employer, or health care clearinghouse; (2) relates to the past, present, or future physical or mental health or condition of an Individual or the past, present, or future payment for the provision of health care to an Individual; and (3) either identifies an Individual or that could be used to identify an Individual, limited to the information created or received by Business Associate from or on behalf of Covered Entity.
“Required By Law” shall mean a mandate contained in law that compels an entity to make a use or disclosure of Protected Health Information and that is enforceable in a court of law.
“Secretary” shall mean the Secretary of the U.S. Department of Health and Human Services or his/her designee.
“Unsecured Protected Health Information” shall mean protected health information that is not secured by a technology standard that renders protected health information unusable, unreadable, or undecipherable to unauthorized individuals and is developed or endorsed by the Secretary or a standards developing organization that is accredited by the American National Standards Institute.
“Breach” shall constitute an impermissible us or disclosure under the Privacy Rule that compromises the security or privacy of PHI.
a. An impermissible use or disclosure of PHI is presumed to be a breach unless the covered entity or business associate, as applicable, demonstrates and jointly determine that there is a low probability that the PHI has been compromised based on a risk assessment of at least the following factors:
i. The nature and extent of the PHI involved, including the types of identifiers and the likelihood of reidentification;
ii. The unauthorized person who used the PHI or to whom the disclosure was made;
iii. Whether the PHI was actually acquired or viewed; and
iv. The extent to which the risk to the PHI has been mitigated.
b. Exceptions to the definition of “breach”
Master Services Agreement
Exhibit A – Business Associate Agreement
i. Unintentional acquisition, access, or use of PHI by a workforce member or person acting under the authority of the covered entity or business associate, if such acquisition , access, or use was made in good faith and within the scope of authority.
ii. Inadvertent disclosure of PHI by a person authorized to access PHI at a covered entity or business associate to another person authorized to access PHI at the covered entity or business associate, or organized health care arrangement in which the covered entity participates.
iii. Covered entity or business associate has a good faith belief that the unauthorized person to whom the impermissible disclosure was made would not have been able to retain the information.
Other terms used in this Agreement, but not defined above shall be defined as they are defined in the HIPAA Privacy Rule.
Section 2. DUTIES
Business Associate agrees to:
a. Limited Use and Disclosure. Not use or further disclose PHI other than as permitted or required by law, as necessary to perform the services set forth in the underlying agreement or by Covered Entity.
b. Prohibition on Sale of PHI. Business Associate shall not directly or indirectly receive remuneration in exchange for any PHI of an individual unless the Covered Entity obtains from the individual a valid authorization that includes a specification of whether the PHI can be exchanged for remuneration by the entity receiving PHI of that individual.
c. Minimum Necessary. Business Associate shall limit its uses, disclosures and requests for PHI to that which is reasonably necessary to accomplish the intended purposes of such use, disclosure and/or request consistent with the Covered Entity’s minimum necessary policies and procedures. Moreover, Business Associate shall disclose the minimum necessary PHI to perform its obligations to the Covered Entity only (i) to its employees, subcontractors, and agents (ii) as directed by Covered Entity; or (iii) as otherwise permitted by the terms of this Agreement.
d. Security and Annual Risk Assessments. Use and maintain appropriate technical, administrative and physical safeguards to prevent use or disclosure of PHI other than as provided by this Agreement and in conformity with Subpart C of 45 CFR Part 164. Business Associate is required to conduct at least an annual security risk assessment and report the results of the risk assessment to Covered Entity.
e. Use of Subcontractors. In accordance with 45 CFR 164.502(e)(1)(ii) and 164.308(b)(2), if applicable, ensure that any subcontractor or agent to whom it provides PHI will agree to the same restrictions, conditions and requirements that apply to Business Associate with respect to such information.
f. Except as otherwise limited in this Agreement, Business Associate may:
(a) use PHI in its possession for the proper management and administration of Business Associate or to carry out the legal responsibilities of Business Associate if such uses are permitted under applicable state and federal confidentiality laws.
(b) disclose PHI to third parties, which are previously informed to Covered Entity, provided that Business Associate obtains reasonable written assurances from such third party that such information shall remain confidential in accordance with the Privacy Rules and shall be used or further disclosed only as required by law or for the purpose for which it was disclosed to such third party, and such third party notifies Business Associate of any instance in which the confidentiality of the information has been breached.
Master Services Agreement
Exhibit A – Business Associate Agreement
(c) Business associate may use PHI to report violations of law to appropriate Federal and State authorities, consistent with §164.502(j)(1).
(d) Business Associate may de-identify PHI received or created pursuant to the underlying Agreement provided that the de-identification process conforms to the requirements of 45 CFR 164.514(b)
g. Reporting of Any Unauthorized Use or Disclosure. Report to Covered Entity, within 5 business days any use or disclosure of PHI of which Business Associate becomes aware that is not provided for in this Agreement, including breaches of unsecured PHI as required at 45 CFR 164.410. The report shall include the identification of each individual whose unsecured PHI has been or is reasonably believed by the Business Associate to have been accessed, acquired, or disclosed during such breach. Notwithstanding the foregoing, for members under the ASES contract (within the Platino population), and in any case of learning of the potential for significant beneficiary harm or situations that may have heightened public or media scrutiny, Business Associate will report to Covered Entity within 24 hours of becoming aware,
h. Access to the Secretary and Covered Entity. Make available its internal practices, books and records relating to the use and disclosure of PHI to Covered Entity and the United States Secretary of Health or its designees for purposes of determining Covered Entity’s compliance with federal rulings such as HIPAA’s Administrative Simplification (Public Law 104-191 enacted on August 1996).
i. Mitigation. Establish procedures to mitigate, to the extent practicable, any harmful effect that is known to Business Associate of a use or disclosure of PHI by Business Associate in violation of the requirements of this Agreement, including the duty to notify affected individuals due to a security breach of unsecured PHI pursuant to §§13401-13402 of the American Recovery and Reinvestment Act of 2009, Public Law 111-5. In this event, the Business Associate agrees to:
a. Provide a full report of the incident to Covered Entity within 48 business hours, and
b. Cover all the costs incurred by Covered Entity as a result of the event
j. Adopt corrective measures if any violation to the terms of the Agreement required by this Article is detected. Covered Entity is authorized to terminate this Agreement if it determines that Business Associate has violated any of its terms.
k. Availability of PHI to Covered Entity. If applicable, make available PHI in a designated record set to the Covered Entity as necessary to satisfy Covered Entity’s obligations under 45 CFR 164.524 to protect the right of the individual to access, inspect and copy his/her PHI.
l. Amendments to PHI. Incorporate any amendments or corrections to PHI in Designated Record Sets when notified and as required by Covered Entity, the individual or his representative that the information is inaccurate or incomplete, pursuant to 45 CFR 164.526.
m. Accounting of Disclosures. Pursuant to 45 CFR 164.528, Business Associate agrees to document and provide to Covered Entity or an Individual, in the time and manner designated by Covered Entity, information disclosed in accordance to the Privacy Rule that must be included in an accounting of Disclosures to permit Covered Entity to respond to a request by an individual for such accounting. Business Associate shall retain such documentation for six (6) years.
Master Services Agreement
Exhibit A – Business Associate Agreement
n. Authentication Process. Institute and maintain procedures that meet the requirements of the Privacy Rule to reasonably verify the identity of an individual requesting access to, or requesting an amendment or an accounting of disclosures.
o. Compliance with Standard Transactions. If applicable, Business Associate will comply and will require any of its subcontractors or agents to comply with each applicable requirement for standard transactions established in 45 CFR Part 162 when conducting all or any part of a standard transaction electronically for, or on behalf of, Covered Entity.
p. If any court or regulatory order or other service of legal process requires Business Associate to disclose information covered by its confidentiality obligations, then Business Associate may make any disclosure required by law. Business Associate will provide Covered Entity with prompt notice of any such order or process prior to the disclosure of any proprietary or confidential information and cooperate with Covered Entity in responding to it.
q. Business Associate represents and warrants to Covered Entity:
(a) that all of its employees, agents, representatives and members of its workforce whose services may be used to fulfill obligations under this Agreement are or shall be appropriately trained as required by the Privacy Rule, and are under legal obligation to Business Associate, by contract or otherwise, sufficient to enable Business Associate to fully comply with all provisions of this Agreement with respect to the Privacy Rule.
(b) that it will reasonably cooperate with Covered Entity in the performance of the mutual obligations under this Agreement with respect to the Privacy Rules.
(c) that it will notify Covered Entity immediately upon becoming aware that any of the foregoing representations and warranties may be inaccurate or may become inaccurate.
Section 3. Obligations of Covered Entity
Covered Entity shall:
(a) Notify Business Associate of any limitations in its Notice of Privacy Practices (under 45 CFR 164.520) to the extent that such restriction may affect Business Associate’s use or disclosure of PHI.
(b) Notify Business Associate of any changes in, or revocation of, permission by an individual to use or disclose PHI, to the extent that such changes may affect Business’s Associate’s use or disclosure of PHI.
(c) Notify Business Associate of any restriction to the use or disclosure of PHI that Covered Entity has agreed to or is require to abide by under 45 CFR 164.522, to the extent that such restriction may affect Business Associate’s use or disclosure of PHI.
(d) Covered Entity shall not request Business Associate to use or disclose PHI in any manner that would not be permissible under Subpart E of 45 CFR Part 164 if done by Covered Entity.
Master Services Agreement
Exhibit A – Business Associate Agreement
Section 4. Inspection and Audit Rights
Covered entity is hereby authorized to conduct inspections of the Business Associate facilities, specifically as it pertains to the protection of PHI and the confidentiality, integrity and availability afforded to the protected health information being held by the Business Associate. Covered Entity reserves the right to perform an audit or security risk assessment on the Business Associate and to require that corrective action plans be created by the Business Associate to remediate the findings.
Section 5. Term and Termination.
Term. The Term of this Agreement shall be effective as of the Effective Date, and shall terminate on the date specified in the underlying agreement or on the date Covered Entity terminates for cause as authorized in this section, whichever is sooner.
Termination for Cause by Covered Entity. A breach by Business Associate of this Agreement is deemed a material breach of the underlying Agreement and as such Covered Entity will notify Business Associate and afford Business Associate an opportunity to cure such breach within thirty (30) days of the Notice of Breach. Failure to cure in the manner set forth under this Section shall constitute grounds for immediate termination of this and any other Agreement. If neither termination nor cure is feasible, Covered Entity shall report the violation to the Secretary.
Termination for Cause by Business Associate. If Business Associate determines that Covered Entity have breached a term of this Agreement, Business Associate may terminate this Agreement upon thirty (30) days notice to Covered Entity of its intent to terminate this Agreement. Business Associate agrees, however, to cooperate with Covered Entity to find a mutually satisfactory resolution to the matter prior to terminating and further agrees that, notwithstanding this section, if it is not feasible to terminate this Agreement so long as an Underlying Agreement is in effect, then Business Associate shall report the problem to the Secretary of the US Department of Health and Human Services, as set forth in 45 CFR 164.504(e)(1)(ii)(B)
Effect of Termination.
(a) Business Associate shall, if feasible, return or destroy all Protected Health Information received from Covered Entity, or created or received by Business Associate on behalf of Covered Entity. This provision shall also apply to PHI that is in the possession of subcontractors or agents of Business Associate. Business Associate shall retain no copies of the PHI, except where return or destruction is infeasible.
(b) In the event that Business Associate determines that returning or destroying the PHI is infeasible, Business Associate shall provide Covered Entity notification in writing, and Business Associate shall extend the protections of this Agreement to such PHI and limit further uses and disclosures of such PHI to those purposes that make the return or destruction infeasible, for so long as Business Associate maintains such PHI.
(i) The Business Associate shall procure to retain only that PHI which is necessary for Business Associate to continue its proper administration or to carry out its legal responsibilities, and return to Covered Entity (or if agreed to by Covered Entity, destroy) the remaining PHI that the Business Associate still maintains in any form. Survival. The obligations of Business Associate under this Section shall survive the termination of this Agreement.
Master Services Agreement
Exhibit A – Business Associate Agreement
Section 6. Miscellaneous Provisions
Notices. All notices, demands, claims, requests, and other communications which may be or are required to be given hereunder or with respect hereto shall be in writing, will either be given by personal delivery, by mail or overnight courier, or by fax, and shall be deemed to have been given or made when personally delivered, and otherwise when received, addressed to the respective PARTIES as follows:
TO COVERED ENTITY:
|
Name:
|
Xxxx Xxxxxxx
|
|
Title:
|
Compliance Officer
|
|
Telephone:
|
(787) 620-1919 ext. 4180
|
|
Fax:
|
(000) 000-0000
|
|
Postal Address:
|
X.X. Xxx 00000 Xxx Xxxx, XX 00000
|
TO BUSINESS ASSOCIATE:
|
Name:
|
Xxxxx X. Xxxxxxxx, M.D.
|
|
Title:
|
CEO
|
|
Telephone:
|
(000) 000-0000
|
|
Email:
|
xxxxxxxxx@xxxxxxxx.xxx
|
|
Postal Address:
|
0000 Xxxxxxxxxx Xxxx Xxxxx, Xxxxxxxx 00000
|
Interpretation. Any ambiguity in this Agreement shall be resolved in favor of a meaning that permits the Parties to comply with the Privacy Rule, federal and local rules or statutes regarding the confidentiality and security of PHI. A reference in this Agreement to a section of the Privacy Rule means the section as in effect or as amended.
Amendments required by law. If HIPAA or other legal requirements relating to the protection of Protected Health Information are instituted mandating an amendment of certain provisions within this Agreement, the Parties agree that this Agreement is amended pursuant to said mandate without further consent of the parties.
Disputes. If any controversy, dispute or claim arises between the Parties with respect to this Agreement, the Parties shall make good faith efforts to resolve such matters informally.
Injunction. Business Associate hereby agrees that Covered Entity will suffer irreparable damage upon Business Associate’s breach of the provisions of this Agreement and that such damages may be difficult to quantify. Business Associate hereby agrees that
Covered Entity may file an action for an injunction to enforce the terms of this Agreement against Business Associate, in addition to any other remedy Covered Entity may have.
IN WITNESS WHEREOF, each of the following undersigned has caused this Agreement to be duly executed.
Covered Entity Business Associate
|
(signed)
|
(signed)
|
|
|
Xxxxxxxx Xxxxxxxxx Xxxxxxx
|
Xxxxxx Xxxxxxxxx
|
|
|
President & CEO
|
Chief Privacy Officer
|
|
|
Triple-S Advantage, Inc.
|
Inovalon, Inc.
|
Master Services Agreement
Exhibit B –Medicare Addendum
Page 1 of 5
EXHIBIT B
Medicare Advantage and Part D Administrative Services
Contract Addendum
This Medicare Advantage and Part D Prescription Drug Plan Contract Addendum (“Addendum”) is issued pursuant to and incorporated by reference in the Master Services Agreement dated January 1, 2016, as amended (the “Agreement”) between, on the one hand, Triple-S Advantage Solutions, Inc., as administrator of Triple-S Advantage, Inc. (collectively the “Company”) and, on the other hand, Inovalon, Inc., on its own behalf and on behalf of each of its affiliates (collectively “Contractor”), hereinafter jointly referred to as the “Parties,” and is effective as of January 1, 2016.
| 1. | Background and Relationship to Agreement |
| 1.1. | The Parties acknowledge that the Centers for Medicare & Medicaid Services (“CMS”) requires that specific terms and conditions be incorporated into the Agreement between a Medicare Advantage Organization and/or Part D Plan Sponsor, such as the Company, and a First Tier Entity, Downstream Entity, or Related Entity, such as Contractor. |
| 1.2. | Provisions of the Agreement that are not inconsistent with this Addendum continue in full force and effect with respect to the services provided pursuant to the Agreement. With respect to the Medicare Advantage line of business, this Addendum shall supersede and replace any inconsistent provisions of the Agreement (or any related agreement) and shall continue concurrently with the term of the Agreement. |
| 1.3. | All capitalized terms used but not defined in this Addendum will have the meaning set forth in the Agreement. |
| 2. | Definitions |
Centers for Medicare and Medicaid Services (“CMS”): The agency within the Department of Health and Human Services (“HHS”) that administers the Medicare program.
Completion of Audit: Completion of audit by HHS, the Government Accountability Office, or their designees of a Medicare Advantage Organization, Medicare Advantage Organization contractor, or related entity related to the services provided under the Agreement.
Downstream Entity: Any party that enters into a written arrangement, acceptable to CMS, with persons or entities involved with the MA benefit, below the level of the arrangement between an MA Organization and a first tier entity. These written arrangements continue down to the level of the ultimate provider of both health and administrative services.
Final Contract Period: The final term of the contract between CMS and the Medicare Advantage Organization.
First Tier Entity: Any party that enters into a written arrangement, acceptable to CMS, with an MA Organization or applicant to provide administrative services or health care services for a Medicare eligible individual under the MA program.
Medicare Advantage (“MA”): An alternative to the Traditional Medicare program in which private plans run by health insurance companies provide health care benefits that eligible beneficiaries would otherwise receive directly from the Medicare program.
Medicare Advantage Organization (“MA Organization”): A public or private entity organized and licensed by a State as a risk-bearing entity (with the exception of provider-sponsored organizations receiving waivers) that is certified by CMS as meeting the MA contract requirements.
Member: A Medicare Advantage eligible individual who has enrolled in or elected coverage through an MA Organization.
Medical Loss Ratio (“MLR”): The medical loss ratio for an MA or Part D plan as described in 42 C.F.R. Part 422, Subpart X and 42 C.F.R. Part 423, Subpart X.
Master Services Agreement
Exhibit B –Medicare Addendum
Page 2 of 5
MLR Reporting Date: The date for each contract year on which the MA Organization or Part D Plan Sponsor reports to CMS its MLR and the data needed to calculate and verify the MLR.
Part D: The Medicare prescription drug benefit administered by private Part D Plan Sponsors under contract with CMS.
Part D Plan Sponsor: A public or private entity that holds a contract with CMS to provide Part D benefits.
Related Entity: Any entity that is related to the MA Organization by common ownership or control and (1) performs some of the MA Organization's management functions under contract or delegation; (2) furnishes services to Medicare enrollees under an oral or written agreement; or (3) leases real property or sells materials to the MA Organization at a cost of more than $2,500 during a contract period.
Traditional Medicare: Means health insurance available under Medicare Part A and Part B through the traditional fee-for service payment system.
| 3. | Requirements |
Contractor agrees to the following:
| 3.1. | Records. The Company, HHS, the Comptroller General, or their designees (either directly or through the Company) have the right to collect, audit, evaluate, and inspect any pertinent information for any particular contract period, including, but not limited to, any operational, financial and administrative records, documentation, books, contracts, computer or other electronic systems (including medical records and documentation of the First Tier Entities, Downstream Entities and Related Entities) directly or indirectly related to the services provided to Company under the Agreement (“Records”) through 10 years from the expiration or termination of the Agreement, or from the date of any Completion of Audit, whichever is later. |
| a. | Contractor will retain all Records for 10 years from the termination or expiration of the Agreement or from the date of any Completion of Audit, whichever is later. |
| b. | Such records must be adequate for the Company to determine if the Contactor has performed its obligations under the Agreement. |
| c. | Such Records must be adequate for the Company to accurately calculate and report its MLR and for the MLR to be validated by CMS. Contractor shall provide all underlying data associated with MLR reporting to the Company upon request, to allow the Company to meet its MLR reporting requirements and CMS validate the MLR. Company agrees to provide Contractor with reasonable notice so that Contractor has sufficient time to respond to any such requests. |
| d. | Contractor must promptly notify the Company by telephone and inform it in writing of any request from any government entity for Records and/or access to personnel, physical premises, facilities, or equipment related to services provided under the Agreement, unless otherwise instructed by HHS, the Comptroller General, or their designees. If permitted by law, Contractor agrees to, upon Company’s request, submit to the Company any such Records requested by the government entity. Contractor agrees to notify the Company of the date and time of any onsite inspection of the Contractor’s premises related to services provided to Company under the Agreement, unless prohibited by government authorities. |
| 3.2. | Member Confidentiality. Contractor will comply with all applicable confidentiality and Member record accuracy requirements, including: (1) abiding by all Federal and State laws regarding confidentiality and disclosure of medical records, or other health and enrollment information, (2) ensuring that medical information is released only in accordance with applicable Federal or State law, or pursuant to court orders or subpoenas, (3) maintaining the records and information in an accurate and timely manner, and (4) ensuring timely access by Members to the records and information that pertain to them. |
| 3.3. | Hold Harmless. Members will not be held liable for payment of any fees that are the legal obligation of the Company. Contractor will not request or accept compensation from a Member for any amounts that are the obligation of the Company, including but not limited to the following circumstances: insolvency of the Company, nonpayment by the Company, or breach of agreement by the Company. |
Master Services Agreement
Exhibit B –Medicare Addendum
Page 3 of 5
| 3.4. | Compliance with CMS Contract. Any services or other activity performed in accordance with the Agreement by Contractor will be consistent and comply with the Company’s contractual obligations to CMS. |
| 3.5. | Compliance with Law. Contractor will comply with all applicable federal, state, and territorial laws, including but not limited to Medicare laws, regulations, and CMS instructions (“Applicable Laws”). |
| 3.6. | Delegation, Revocation, and Monitoring. Company is delegating certain of Company’s activities or responsibilities under its contract with CMS, as described further below: |
| · | The delegated activities and reporting responsibilities of Contractor are specified in the Agreement. |
| · | CMS and the Company (including the Company acting at its own discretion in the absence of CMS involvement) reserve the right to immediately revoke, in whole or in part, the delegation of the services to be provided under the Agreement and associated reporting requirements or to specify other remedies in instances where CMS or the Company determine that such parties have not performed satisfactorily. |
| · | The Company is ultimately responsible for performance under its contract with CMS and will monitor the performance of Contractor under the Agreement on an ongoing basis. Contractor agrees to cooperate fully with the Company’s monitoring and auditing program. |
| 3.7. | No Exclusion or Debarment. Contractor represents and warrants that it and its employees, contractors, governing body members, and any Downstream Entities are not excluded or debarred by the HHS Office of Inspector General or by the General Services Administration from participation in any federal health care program, and that they are not, to the best of Contractor’s knowledge, under investigation for any such exclusion or debarment. Contractor agrees not to use federal funds to pay for work or services provided by a provider, employee or Downstream Entity excluded by the Department of Health and Human Services’ Excluded Individuals and System for Award Management (formerly Entities List or the General Services Administration’s Excluded Parties Lists System). Contractor must review the lists prior to hiring or contracting a new employee or entity and supplemental/update files must be reviewed on a monthly basis. Contractor will notify Company immediately if there are any changes in status under this paragraph. Contractor acknowledges that the Agreement and/or any SOW under the Agreement for the provision of the delegated services may be terminated immediately if Contractor is excluded from participation in any federal health care program. |
| 3.8. | Subcontracting. Contractor will not contract with any entity to perform the delegated services to be provided under the Agreement unless (a) such arrangement is made in accordance with the terms of the Agreement; (b) such person or entity is obligated, through a written agreement executed between such entity and Contractor, to comply with all of the provisions contained in the Agreement between Company and Contractor; and (c) such written arrangement specifically permits the Contractor to terminate the delegation if such entity breaches the delegation agreement between the entity and Contractor. |
| 3.9. | Credentialing. To the extent that Contractor performs healthcare provider credentialing services, the credentials of medical professionals credentialed by or affiliated with Contractor will be either reviewed by the Company or the Contractor’s credentialing process will be reviewed and approved by the Company. The Company will audit the credentialing process on an ongoing basis. In addition, to the extent that the Company delegates the selection of healthcare providers or subcontractors, the Company retains the right to approve, suspend, or terminate any such arrangement. |
| 3.10. | Data that Determine Payment. To the extent that Contractor generates data used to determine payment by CMS, including but not limited to calculation of the Company’s MLR or used to identify possible overpayments, such as information on enrollment of Members, encounter data, claims data, data relating to the Company’s bids submitted to CMS, or other data specified by the Company or CMS, Contractor will certify that such data are complete, truthful, and accurate and will make this certification (a) to the Company, and/or (b) directly to CMS, when required by the Company, by Applicable Law, or CMS. |
Master Services Agreement
Exhibit B –Medicare Addendum
Page 4 of 5
| 3.11. | Federal Funds. Contractor acknowledges and agrees that payment for the services provided under the Agreement is made, in whole or in part, from federal funds. |
| 3.12. | Off-Shore. In performing services under the Agreement, Contractor will not perform any functions, activities or services (or directly or indirectly contract with any person or entity that performs any functions, activities or services), including, without limitation, access to or storage of Member information, outside of the United States of America or its territories without the prior written consent of the Company. |
| 3.13. | Training and Compliance. Contractor agrees to: |
| · | Ensure that all personnel (including contractors) involved in the performance of the services provided under the Agreement (i) complete the compliance and fraud waste and abuse training module required by CMS (the “CMS Module”) and (ii) receive specialized Medicare Advantage and Part D compliance training pertaining to their duties. This training must be provided initially upon hiring, and annually thereafter, as a condition of employment and must comply with all Applicable Laws pertaining to training, including but not limited to the requirements set forth in the CMS Compliance Program Guidelines (contained in the Medicare Managed Care Manual as Chapter 21 and in the Prescription Drug Benefit Manual as Chapter 9) (the “Compliance Program Guidelines”). Contractor must be able to provide certificates of completion for all individuals taking the CMS Module at least annually to the Company, and upon request by the Company or CMS. |
| · | As appropriate to Contractor’s organization and the nature of the services provided under the Agreement, establish and maintain an effective compliance and anti-fraud program to ensure compliance with Applicable Laws and to detect and prevent the incidence of fraud, waste and abuse relating to the provision of the services. Such program will meet the requirements of 42 C.F.R. §§ 422.503(b)(4) (vi) and 423.504(b)(4) (vi) regarding effective compliance programs. Contractor will notify promptly its authorized representative at Company of any instance of noncompliance or misconduct related to Company’s Medicare Advantage program. |
| · | Cooperate with the Company in any investigation that the Company, in its sole discretion, conducts in connection with the Company’s compliance or fraud, waste, and abuse programs directly or indirectly related to the Agreement. |
| · | Contractor agrees that it and its personnel will comply with all applicable Company policies and procedures (access to which has been provided to Contractor), including but not limited to any Company Standards of Conduct. |
| · | Contractor agrees upon reasonable request to formally attest to meeting the training and compliance and anti-fraud program obligations described in this Addendum. |
| 3.14. | Amendments. Company may amend this Addendum upon 30 days' notice, unless an earlier effective date is required by rule or regulation, to Contractor solely to conform this Addendum to any changes to applicable laws, regulations, or CMS requirements or instructions. Any other amendments will be in writing signed by the Parties. |
Master Services Agreement
Exhibit B –Medicare Addendum
Page 5 of 5
IN WITNESS WHEREOF, the Parties have signed this Addendum is effective as of the Effective Date defined herein.
|
Triple-S Advantage Solutions, Inc.
|
Inovalon, Inc.
|
|||
|
By:
|
/s/ Xxxxxxxx Xxxxxxxxx Xxxxxxx
|
By:
|
/s/ Xxxxx Xxxxxxxx | |
|
Name:
|
Xxxxxxxx Xxxxxxxxx Xxxxxxx
|
Name:
|
Xxxxx Xxxxxxxx, M.D. | |
|
Title:
|
President & CEO |
Title:
|
CEO | |
|
Date:
|
November 6, 2015 |
Date:
|
November 6, 2015 | |
Master Services Agreement
Exhibit C – Report Inventory
EXHIBIT C
Report Inventory
|
Inovalon, Inc.
Inovalon Report Schedule
Date: 11/03/2015
|
 |
|
Product
|
Report Type
|
Location
|
Frequency
|
|
CAAS
|
901 CAAS Impact Report (Following complete CMS RAPS Return Files)
|
American Health Medicare>>CAAS>>2015>>June>>2015 DOS
|
Monthly
|
|
CAAS
|
910 RAPS Attribution (Following complete CMS RAPS Return Files)
|
American Health Medicare>>CAAS>>2015>>June>>2015 DOS
|
Monthly
|
|
CAAS
|
920 RAPS Errors (Following complete CMS RAPS Return Files)
|
American Health Medicare>>CAAS>>2015>>June>>2015 DOS
|
Monthly
|
|
CAAS
|
935 Encounter Deactivation
|
American Health Medicare>>CAAS>>2015>>June>>2015 DOS
|
Monthly
|
|
CAAS
|
937 Provider Eligibility
|
American Health Medicare>>CAAS>>2015>>June>>2015 DOS
|
Monthly
|
|
XXXX
|
Xxxxxxxx Reporting - Diagnoses captured in chart reviews that are in quality process and are yet to be scored or submitted in RAPS for TSS 2014 DOS
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
XXXX
|
Xxxxxxxx Reporting - Diagnoses captured in chart reviews that are in quality process and are yet to be scored or submitted in RAPS for AHM 2014 DOS
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
CARA
|
405 CEDI Process Summary Reporting
|
INDICES and American Health Medicare>>CARA>>2015 RRO>>Opportunity Reports
|
Prior to Launch of each CARA Process
|
|
CARA
|
410 CEDI Opportunity Details
|
INDICES and American Health Medicare>>CARA>>2015 RRO>>Opportunity Reports
|
Prior to Launch of each CARA Process
|
|
CARA
|
431 Report - All Sites
|
American Health Medicare>>CARA>>2015 RRO>>Complete Chase List
|
Prior to Launch of each CARA Process
|
|
CARA
|
310 Financial Impact
|
INDICES
|
After the close of each process
|
|
CARA
|
Realization Reports
|
INDICES
|
After the close of each process
|
|
CARA
|
Key Impact Reports
|
INDICES
|
After the close of each process
|
|
CARA
|
MRR Update
|
email
|
Weekly
|
|
CARA
|
RAPS Files
|
FTP
|
2nd Friday of each month
|
|
PA
|
RAPS Files
|
FTP
|
3rd Thursday of each month
|
|
PA/CARA
|
5010 Files
|
American Health Medicare>>Communications>>EDPS Files 2015 xxx
|
3 business days following RAPS delivery
|
|
PA
|
MMDM Files - PA Measure
|
American Health Medicare>>Star Advantage>>MMDM Summary Reports>>2015
|
Monthly (Due by 4th week of each month)
|
|
PA
|
MMDM Files - PA Measure Members
|
American Health Medicare>>Star Advantage>>MMDM Summary Reports>>2015
|
Monthly (Due by 4th week of each month)
|
|
PA
|
MMDM Files - PASA Summary
|
American Health Medicare>>Star Advantage>>MMDM Summary Reports>>2015
|
Monthly (Due by 4th week of each month)
|
|
PA
|
Milliman Reporting - PA Volume Tracker
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
PA
|
Milliman Reporting - RAPS submitted to TSA for 2015 DOS.
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
PA
|
Milliman Reporting - Diagnoses captured in ePASS tool for 2015 DOS that are yet to be scored
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
PA
|
322 Financial Impact Summary
|
INDICES
|
Quarterly
|
|
PA
|
510 Factor Impact Member Listing
|
INDICES
|
Quarterly
|
|
PA
|
520 HCC Impactful Gaps Summary
|
INDICES
|
Quarterly
|
|
PA
|
530 HCC Gap Closure Member Detail
|
INDICES
|
Quarterly
|
|
PA
|
IP-010 Data Report
|
email
|
Monthly
|
|
PA
|
IHA Dashboard
|
American Health Medicare>>Custom Analyses>>2015>>IHA Dashboards>>June
|
Weekly
|
|
PA/XXXX
|
Xxxxxxxx Reporting - RAPS submitted to TSA for TSS 2014 DOS
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
PA/XXXX
|
Xxxxxxxx Reporting - RAPS submitted to TSA for AHM 2014 DOS
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
PA/XXXX
|
Xxxxxxxx Reporting - Data Dictionary
|
American Health Medicare>>Custom Analyses>>2015>>Monthly Tracking>>June
|
Monthly (Due by 1st week of each month)
|
|
SA
|
Pseudocode File
|
American Health Medicare>>Star Advantage>>Pseudo Codes>>2015
|
Monthly
|
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 1 of 16
Statement of Work #1
PROSPECTIVE MEDICARE ADVANTAGE RISK ADJUSTMENT
(Known as Prospective Advantage® services)
This Statement of Work #1 (this “SOW”) is entered into and effective as of the Effective Date (the “SOW Effective Date”) of that certain Master Services Agreement effective January 1, 2016 (as amended, the “Agreement”) by and between Inovalon, Inc. and Client pursuant to the terms and conditions thereof. Inovalon will use all commercially reasonable efforts to provide the following Prospective Advantage® services (the “Services”) to Client in a professional and workmanlike manner.
| 1. | Definitions. For the purposes of this SOW, the following terms are defined as follows: |
| a. | “Member Population” shall mean the group of members comprised of the enrollees within the Medicare Advantage product line of Client for which Services are to be rendered, as designated by Client. Inovalon and Client agree that Inovalon will be the sole third party vendor only for the provision of the contracted Services for the Member Population as outlined in this SOW. With respect to the Member Population, Client may, at its discretion, complement or pursue additional initiatives using other contractors, but, Client agrees to share with Inovalon the results of any such complementary services. For clarity, such complementary services will not be in lieu of or decrease from the Services provided by Inovalon. Additionally, nothing in this definition prevents Client from revoking delegated Services in the event of a breach on the part of Inovalon. Client shall supply Inovalon with identifying information for those individual members included in the Member Population. Client has the right to exclude Medicare Advantage members from the Member Population, subject to the limitations described below. Client will ensure that the Member Population meets the minimum requirements listed below. Client will define the Member Population by providing Inovalon with written notice of a preliminary percentage estimate by October 1st preceding the applicable calendar year, a final percentage by November 1st preceding the applicable calendar year, and the actual members within the Member Population within one week of December 7th preceding the applicable calendar year. The parties acknowledge that the flexibility to define the Member Population may affect the ability of Inovalon to meet certain return on investment provisions in a particular SOW, and this will be taken into consideration when measuring the return on investment requirements. The Member Population as defined herein applies only to Encounter Facilitations and Supplemental Member Encounters. The Member Population for Encounter Support as described in Section 6(b) of the SOW and the analytics described in Section 5 of the SOW is defined as all unique members enrolled in all health plans within any applicable product line of Client during the applicable date of service period for which the Services are rendered, including plans acquired through corporate transactions or otherwise. |
| i. | For the calendar year 2016, the Member Population shall be comprised of no less than sixty-five percent (65%) of Client’s total then-current Medicare Advantage membership. |
| ii. | For the calendar year 2017, the Member Population shall be comprised of no less than fifty-five percent (55%) of Client’s total then-current Medicare Advantage membership. |
| b. | “Health Plan Data Set” shall mean data files for each Member Population, as provided from Client to Inovalon in their raw native format, including: member demographics, member product enrolment segments, known member hierarchical condition category and factor data (HCC, CRG, CDPS, or other risk adjustment categorization data, as the case may be), CMS (e.g., MOR, MMR, RAPS, RAPS Return, EDS, and Bid files, in the case of Medicare Advantage, as the case may be) or State Department of Health risk adjustment files (e.g., MEDS II, eData, Bid files, and other such similar risk adjustment and reporting files, in the case of State Managed Medicaid, as the case may be), and provider demographics, provider service claims, provider encounters and diagnoses, member laboratory results, pharmaceutical prescription claims, durable medical equipment claims, and public data repository and registry files. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 2 of 16
| c. | “Authorized Users” shall mean those providers and support staff who are identified by Client as being authorized to use the ePASS™ solution. |
| d. | “Predictive Clinical Insight System” (PCIS™) shall mean that set of proprietary, clinically-driven algorithms used to identify data which suggests evidence of gaps in documentation, assessment, or care considerations (e.g., quality or clinical care). It is through this process, amongst others, that Inovalon identifies clinical areas of care, coordination, documentation, and outcomes improvement opportunities. PCIS is a proprietary process and is a component, along with all proprietary data sets utilized thereby, of Inovalon Intellectual Property. |
| e. | “Documentation Gaps” shall mean a clinical encounter data incongruence (CEDI™) which is identified during the analysis of Health Plan Data Sets through the application of Inovalon’s PCIS suggesting the existence of chronic, additional, worsening, or more optimally classified disease and/or co-morbidity processes not already documented within the standard administrative claims system of Client or not otherwise coded within formats appropriate for submission to CMS or state health departments, as the case may be (e.g., it is believed that a member has an active condition for which such member has been seen and assessed but appropriate reflection of such active condition is absent or invalid within Client’s administrative claims systems). |
| f. | “Assessment Gaps” (UnCoded Chronic Condition or UCCC™) shall mean an enrollee’s (or member’s) of a Client health plan condition identified to be present through the application of Inovalon’s PCIS as having claims or encounter data consistent with one or more chronic conditions on a historical basis, except for the absence of an eligible documented encounter during a relevant date of service period that is under review (e.g., it is believed that a member has a historical and expectedly still active condition for which current assessment is believed to be lapsing). |
| g. | “Care Consideration Gaps” shall mean a medication, laboratory, procedure, outcome, resource utilization, or other member care issue that is identified as potentially having occurred or not occurred such that best practice, utilization improvement, quality measure, or safety standards may have been jeopardized (e.g., it is believed that a member has been maintained on a specific medication without having blood levels checks at appropriate intervals, or it is believed that a member for whom a breast cancer screening mammogram should have been performed and for which no evidence can be identified, per “best practice” standards). |
| h. | “Smart HRA™” shall mean a health risk assessment which is dynamically customized to reflect the known medical data pertaining to a specific member, thereby curtailing the assessment to focus on matters for which clarifying data is sought and avoiding unnecessary questions for data which is already known. The Inovalon Smart HRA toolset is incorporated within the ePASS solution to facilitate the data-driven achievement of a dynamic Encounter SOAP used to identify, close or clarify the validity or status of Documentation Gaps, Assessment Gaps, and Care Consideration Gaps (collectively, “Prospective Advantage Gaps”). |
| i. | “ePASS Portal” shall mean the internet-based secured web portal developed and maintained by Inovalon which provides Authorized Users and Member Assessors (as defined below) with access to certain reports and analytical tools regarding their respective patients. |
| j. | “Member Disease State Profile” shall mean the set of all known disease conditions eligible for CMS or State Department of Health reimbursement under the HCC CRG, CDPS, ACG, or DxCG, as the case may be, coding system for a specific member, as well as relevant supporting data and associated encounter and/or claim dates. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 3 of 16
| k. | “Encounter SOAP Note” shall mean the documentation employed by providers to document a face-to-face patient assessment. |
| 2. | Term and Termination. This SOW shall commence on the Effective Date of the Agreement and shall continue through December 31, 2017. |
| a. | Termination Option in the Event of Demonstration of Limited Benefit. Provided Client has elected to utilize all three available PA Gap Resolution & Closure Processes and has reasonably satisfied its obligations hereunder, Client will have a right to terminate this SOW (a) January 31, 2017 (the “Initial Termination Option Date”), and (b) the date of each anniversary of the Initial Termination Option Date (each, an “Annual Termination Option Date”) (the Initial Termination Option Date and each Annual Termination Option Date referred to as a “Termination Option Date”), in the event that the aggregate reimbursement improvement resulting from the Services does not exceed three times the cost of the total fees paid to Inovalon with respect to such corresponding Services, calculated as the total financial impact as evidenced in Inovalon’s impact tracking reports (described below). Each successive termination right will expire upon the earlier of (i) 15 days after the respective Termination Option Date, or (ii) the date Client notifies Inovalon of its desire to continue with the Services contemplated herein. For the avoidance of doubt, in the event that Client does experience aggregate reimbursement improvement resulting from the Services hereunder in excess of three times the cost of the total fees paid to Inovalon with respect to such corresponding Services, or as each limited termination right provided under this Section 2 expires, the term of this SOW will remain in effect and such termination right will become null and void. |
| b. | Transition Services. In the event of termination or expiration of the Agreement and with respect to Client’s Medicare Advantage members who will no longer be part of the Member Population effective January 1 of a contract year in accordance with the process outlined in Section 1(a) of this SOW, Inovalon will provide the support described below up until the end of the Transition Period (as defined below) both (A) in accordance with all standards set forth in the Agreement and this SOW and (B) with the same level of accuracy, intensity and timeliness of Services performed before receipt of the notice of termination or non-renewal, meeting all the data specifications required by Client and CMS. In consideration of the transition services, Inovalon will continue to invoice and Client will continue to pay the Base Processing Fee described in Section 9(a) of the SOW during the 3 month period following (a) the Termination Date or (b) January 1 with respect to Client’s Medicare Advantage members who are no longer part of the Member Population in accordance with the process outlined in Section 1(a) of this SOW (the “Transition Period”). Notwithstanding the foregoing, in the event of a termination under Section 1.2(i) of the Agreement, Inovalon will not invoice and Client will not be obligated to pay the Base Processing Fee described in Section 9(a) of the SOW during the Transition Period. |
| i. | Inovalon will keep the ePASS portal open and available until the end of the Transition Period; |
| ii. | Inovalon will continue to review and code all Member Assessment SOAP Notes received through ePASS until the end of the Transition Period; |
| iii. | Inovalon will complete, code and create corresponding RAPS files and EDS files for all Face-To-Face Member Assessment scheduled prior to the Termination Date during the Transition Period; |
| iv. | Inovalon will complete all Encounter Facilitation outreach initiated prior to the Termination Date and will complete such interventions during the Transition Period with no new Encounter Facilitations being initiated following the Termination Date; |
| v. | Inovalon will make available to Client all Member Assessment SOAP Notes received through ePASS or created as part of a Face-To-Face Member Assessment by the end of the Transition Period; and |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 4 of 16
| vi. | Inovalon will complete all Encounter Facilitation mailings within the Transition Period. |
| 3. | Project Initiation Activities & General Project Management. Inovalon will undertake the following steps: |
| a. | Project Integration Call: Inovalon will schedule and coordinate a project integration call with Client during which the following materials and topics will be provided, introduced, and addressed: |
| i. | Inovalon Contact Information: Team contact information for primary Inovalon project personnel and support escalation protocols will be provided to Client; |
| ii. | Project Plan: A comprehensive Project Plan will be reviewed with Client which will include overall process timelines, data delivery and deliverable schedules, and ongoing team collaboration recommendations scheduling for both Client and Inovalon; and |
| iii. | Project Questionnaire: A questionnaire identifying key information requirements by Inovalon of Client (such as the clarification of Client IT personnel contact information, database characteristics, and other such applicable details) will be provided by Inovalon to Client with mutually agreed upon follow-up completion and timeline details. |
| b. | System Training: Inovalon will schedule, coordinate, and conduct solution training for designated Client personnel consisting of instructions for accessing: |
| i. | Client Web Portal functions; |
| ii. | Threshold selection; and |
| iii. | Process Reporting. |
| c. | Establish Joint Implementation Schedule: Based on the information gained from the Project Integration Call (Section 3(a) above) and information returned to Inovalon within the Project Questionnaire, Inovalon will establish and conduct a mutually agreed upon comprehensive schedule for conference calls (generally bi-weekly ) for, amongst other issues, the: |
| i. | Provision of project status reports; |
| ii. | Review and reconciliation of Project Plan activities; |
| iii. | Review of issue tracking reports (if any) and respective resolution status; and |
| iv. | Identification and discussion of new issues for resolution (if any). |
| d. | Specification of Data Requirements: Inovalon shall provide to Client a data specification document (referred to as the Inovalon Data Specification Document, as referenced within the Health Plan Data Set definition above). Based on the information gained from the Project Integration Call (Section 3(a) above) and information returned to Inovalon within the Project Questionnaire, Inovalon will provide Client with any supplemental specifications, the sum of which shall serve as a comprehensive outline of data required by Inovalon for the administrative data processing of each Member Population (which will constitute components of the Health Plan Data Set for each Member Population) including, amongst other data, the: |
| i. | Member demographics data; |
| ii. | Member claims and cost data; |
| iii. | Member enrollment data; |
| iv. | Member laboratory data; |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 5 of 16
| v. | Member pharmacy data; |
| vi. | Member procedure data; |
| vii. | Member durable medical equipment data; |
| viii. | Payment agent-specific data such as: |
| 1. | Medicare Advantage data such as: |
| A. | RAPS & RAPS Return data and EDS data; |
| B. | MOR Detail data; |
| C. | MMR Detail data; |
| D. | CMS Bid Data; |
| 2. | Managed Medicaid data such as: |
| A. | Electronic submission file data (e.g. MEDS II, eData, etc.); |
| B. | State Bid, Factor, and Rate data; |
| 3. | Commercial data such as: |
| A. | Monthly premium data. |
| ix. | Care provider data; and |
| x. | Other such data which may be relevant to the practice, utilization, and cost data of the members and providers within the Member Population. |
| e. | Approval of Member and Provider Communications. Inovalon shall provide to Client the forms and/or general content of proposed talking points and letters to be distributed to members and/or providers, as applicable. Recognizing that time is of the essence, Client shall apply all reasonable efforts to make any revisions reasonably necessary (if any) within 10 business days in order to maintain project timelines. |
| 4. | Data Transfer and Transform Processing; Maintenance of Client Data Repository. Inovalon shall implement a data integration and refresh/update in association with each monthly processing cycle. |
| a. | Inovalon shall allocate and dedicate datacenter infrastructure, administration, security, and oversight resources necessary to receive, process, and maintain all Health Plan Data Sets (the “Client Data Repository” or “CDR”). |
| b. | Inovalon will work with designated Client personnel in their provision of a secure and complete Health Plan Data Set from Client to Inovalon’s designated CDR via FTP using established, industry standard transfer, compression, and encryption protocols. |
| c. | Inovalon and Client will establish a transfer schedule for ongoing provision of the Health Plan Data Set (occurring no less than monthly) in order to allow for the timely application of the disease, comorbidity, and gap identification algorithms within each monthly process cycle. The first Health Plan Data Set shall be provided by Client to Inovalon within 5 business days of the SOW Effective Date. Client will provide Medicare Advantage membership files for processing at least weekly, and Inovalon agrees to accept these files and to work to update ePASS with the new files for no additional charge. |
| d. | Data received from Client will be tagged, tracked, and staged into the CDR by Inovalon in its raw formats in order to allow for full source file attribution, audit trail, and mapping reconciliations. |
| e. | Client must notify Inovalon (before the provision of such) of any change to Client’s raw formats so as to facilitate accurate and efficient integration into the CDR. |
| f. | Inovalon shall facilitate all necessary data translations, crosswalks and mapping into the CDR, evaluating for consistency with expected values (referred to, amongst other analysis, as the “Integrity Analysis”). |
| g. | Both parties acknowledge the importance of partnership and the presence of mutual responsibilities with respect to data and its exchange. As such: |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 6 of 16
| i. | Inovalon and Client will jointly review, validate, and approve the translations, crosswalks, and mapping protocols of raw data to facilitate the accurate loading and maintenance of the CDR; |
| ii. | Inovalon will work with designated Client personnel to resolve data inconsistency, data gaps, and data value validation issues and to facilitate appropriate data source matching and reconciliation; and |
| iii. | Client shall be responsible for providing to Inovalon all data needed (and in a timely fashion) for the provision of these Services and will notify Inovalon if Client becomes aware of missing, incomplete, changed formats, late, or erroneous data. |
| 5. | Service Segments. Inovalon shall provide services (the “Prospective Advantage Services”) to Client consisting of the analytics described in this Section 5, designed to achieve a comprehensive prospective approach to identifying and prioritizing resolution to gaps in assessment, documentation, and quality. |
| a. | Project Management: Each party shall appoint an employee to serve as the primary point of contact with the other party in connection with this SOW (for each party, the “Project Manager”). Each party may change its Project Manager upon written notice to the other party. In the event that Client is dissatisfied with Inovalon’s appointed Project Manager and reasonable good faith efforts by both parties have failed to resolve such dissatisfaction, Inovalon shall appoint a different Project Manager and achieve the transition to such replacement Project Manager along a timeline which is mutually agreed to by the parties. |
| b. | Monthly Analytics. Inovalon shall, on a monthly basis, apply its algorithms to Health Plan Data Sets to perform analysis of member historical clinical patterns, disease, and co-morbidity states (including for both the previous and current calendar years) to identify members with Prospective Advantage Gaps and therefore without any, or without adequate, claims and risk adjustment impact coding, during the then current calendar year (the “Current DOS Period”). For each monthly process, Inovalon shall undertake the following: |
| i. | Identification of Prospective Advantage Gaps: |
| 1. | Identify Documentation Gaps per the application of Inovalon’s Predictive PCIS designed to determine the identification of members possessing clinical indications of disease and co-morbidity states not otherwise present within Client administrative claims data systems, otherwise known as Clinical Encounter Data Incongruences (each a “CEDI”), the probability and factor score thresholds of which shall be determined and set upon review of Member Population data by Inovalon. |
| A. | Provided that Client is concurrently engaged with Inovalon’s CARA™ solution, all CEDI Documentation Gaps shall be integrated from the respective CARA processes and no duplication of such processes or associated CEDI identification fees shall be applied. |
| 2. | Identify Assessment Gaps per the application of Inovalon’s PCIS designed to determine the identification of members possessing historical indications of chronic disease (or such medical conditions which may be expected to be persistent in nature) and for which a valid clinical encounter and associated valid claim is not able to be identified within the current date of service period per the CMS (or State Department of Health, as the case may be) technical specifications of risk adjustment, otherwise known as Un-Coded Chronic Conditions (each a “UCCC”), the probability and factor score thresholds of which shall be determined and set upon review of Member Population data by Inovalon. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 7 of 16
| 3. | Identify Care Consideration Gaps per the application of PCIS designed to determine the identification of members with data suggesting potential medication, laboratory, procedure, outcome, resource utilization, or other patient care issue that is identified as potentially having occurred or not occurred such that best practice, utilization improvement, quality measure, or safety standards may have been jeopardized. |
| ii. | Venue Assessment Analytics: Inovalon shall undertake the analytical algorithms necessary to determine effective interventional approach with respect to venue for prospective closure of each member identified as having one or more Prospective Advantage Gaps as outlined above. Such venue analytics shall be utilized to direct intervention strategy regarding selection of encounter facilitation, encounter support, and in-home (or face-to-face) assessment for the closure and resolution of such gaps. |
| iii. | Gap Coordination Analytics: For each member for whom gaps in assessment, documentation, and care and quality have been identified, Inovalon shall undertake an analytical process of determining the following: |
| 1. | Gap Prioritization: Recognizing that resource planning requires a prioritization of implementations over time, gap prioritization is necessary to balance intervention loads. |
| 2. | Provider Selection: The effectiveness of gap closure is impacted by the type of provider and nature of the provider’s relationship with a respective member in the setting of a specific gap type. Provider selection algorithms undertake a consideration of factors influencing the likelihood of a gap closure intervention being successful when undertaken in concert with a specific provider. |
| 3. | Closure Method Selection: The effectiveness of gap closure is impacted by the method applied to close such gap (e.g. encounter facilitation, encounter support, or Face-To-Face Member Assessment). Closure method selection algorithms undertake a consideration of factors influencing the likelihood of a gap closure intervention being successful based on the clinical encounter data of the respective member, the nature of the Prospective Advantage Gaps, and the providers identified within the Provider Selection algorithms. |
| 4. | Overlap & Sequencing: Prospective Advantage Gap closure can be made more efficient by coordinating multiple Prospective Advantage Gaps identified. Prospective Advantage Gaps of lower potential value or with less pressing timing priority may best be coordinated with Prospective Advantage Gap of higher potential value or more timely need for closure. Overlap and sequencing algorithms determine a method of more efficient grouping and chronology of Prospective Advantage Gap closure intervention to achieve efficient balancing of timing, efficiency, and value. |
| c. | Creating and Updating of Target Gap Set & Mapping. Inovalon shall, on a monthly basis, determine the then current set of Prospective Advantage Gaps from the results derived from the analytical process outlined within Section 5(b) above, providing for a current and forward looking indication of relevant gaps, recommended method and venue of closure, sequencing, and timing so as to assist in gap resolution and closure (for each month, the respective “Prospective Advantage Monthly Member Detail Map” or “Prospective Advantage MMDM”). Such Prospective Advantage MMDM shall be reflective of actual clinical and encounter activity (as reflected within the Health Plan Data Set) of the immediately preceding month, making adjustments to gap, venue, and coordination analytical results upon preceding Prospective Advantage MMDM data to reflect such. |
| 6. | Gap Resolution and Closure. Guided by the results analytics described above, Inovalon will implement a process of gap resolution and closure (the “PA Gap Resolution & Closure Processes”) through a combination of encounter facilitation, encounter support, and in-home assessment. Such PA Gap Resolution & Closure Processes shall be undertaken as outlined in this Section 6. If any of Client’s members decline to receive any contact from Inovalon, Inovalon will inform Client of such member refusals on a monthly basis. Inovalon will operationalize a process to inform Client of such member refusals on a weekly basis. Member complaints will be escalated to Client within two business days. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 8 of 16
| a. | Encounter Facilitation: For each member identified as being in need of encounter facilitation for gap resolution and closure, Inovalon shall undertake a coordinated communication outreach process to facilitate encounters with the respective provider to achieve appropriate member assessment, documentation, coding, risk adjustment accuracy, care and quality gap resolution. Inovalon will manually adjust the PA Gap Resolution & Closure Process so that no Encounter Facilitations will be launched during the months of July or December unless otherwise agreed upon the parties. |
| i. | Member Outreach: Inovalon will outreach to members in writing and telephonically with information regarding the recommended need for a provider assessment (without specific disease information) and provider contact information in such a manner, as to facilitate timely practitioner encounter. |
| ii. | Provider Outreach: Inovalon will outreach to providers in writing with information regarding the recommended need for a provider assessment of one or more specific members (with specific gap information) and relevant member contact information to facilitate a timely practitioner encounter. |
| 1. | Enhanced Provider Outreach. In the event that the Encounter Support Gap Resolution Modality is not in place, a relevant provider does not have ready access to (or is not readily adopting of) ePASS, or in an effort to more effectively achieve the benefits of comprehensive documentation of encounters, Inovalon may additionally provide a member-specific encounter SOAP (Subject Objective Assessment Plan) note to providers in connection with the provider outreach of Section 6(a)(ii) and request submission to Inovalon of such completed Member Assessment SOAP Notes. Upon the receipt, analysis/review, coding, and processing of such Member Assessment SOAP Note, an Encounter Support shall have been deemed to have been successfully undertaken (as opposed to an Encounter Facilitation, and such Encounter Support shall also be referred to as a “Converted Encounter Facilitation”). |
| b. | Encounter Support: So as to facilitate a highly effective provider encounter aimed at resolving and closing gaps, (i.e. clarifying to providers where specific gaps exist at the time of encounters with such members), Inovalon shall provide encounter support for providers and their members consisting of member data insight, targeted member assessment & documentation support for members identified as having gaps (a process component referred to as the “Encounter Support Process”) through a service platform referred to as the Electronic Patient Assessment Solution Suite (ePASS®) or through the provision of a printed form of materially the same content if directed by Client (i.e. for those Clients not desiring or not able to utilize an electronic platform, whether universally or on a provider-by-provider basis). For each Encounter Support Process, Inovalon shall undertake the following: |
| i. | Notification to Providers. On a monthly basis, Authorized Users are reviewed by Inovalon such that: |
| 1. | Authorized Users who are new to the Encounter Support ePASS solution are provided general ePASS materials and offered access to technical support and training materials; and |
| 2. | A list of all members who have been identified as having a Documentation Gap, Assessment Gap, and/or Care Consideration Gap and who are within such provider’s Provider Viewable Membership list (as defined below) receive notification of such with detail indicating the suspicion of such gaps. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 9 of 16
| ii. | Notification to Members: All members who are identified as having a suspected Documentation Gap, Assessment Gap, or Care Consideration Gap shall receive a letter (or other textual communication including for example email and SMS) with prioritized members additionally receiving facilitating telephonic outreach which: |
| 1. | References the value of appropriate medical follow-up with their provider (but does not state the specific area of potential Documentation, Assessment, or Care Consideration Gap); and |
| 2. | Contains information designed to assist the member in pursuing an appropriate encounter with the designated provider. |
| iii. | Information & Support in Encounters: Member encounters supported by the ePASS platform of the Encounter Support Process provide Authorized Users gain the benefit of: |
| 1. | Member Electronic Healthcare Data Records: Member data pertaining to demographics, risk adjustment (HCC, ACG, CRG, DxCG, CDPS, or other such similar risk adjustment model detail) data, past medical history, encounter data, laboratory data, pharmacy data, durable medical equipment data, care provider data, and other such data is provided in a “read-only” electronic medical record format from which the provider can gain advantageous insights into the member’s medical history, tests, and treatment so as to assist in their assessment, documentation, decision making, and care plan construction processes. |
| 2. | Smart HRA (Health Risk Assessments) Decision Support / Leading Question Guidance: Questions that are based on indications of Prospective Advantage Gaps and other relevant data aid in clarifying the presence, persistence, and status (or absence or evolution) of the active medical conditions and potential co-morbidities (and the documentation and clarification of such). |
| 3. | Improved Documentation & Data Clarity: Following the completion of each ePASS-supported encounter hereunder, Authorized Users and Client are provided a: (i) detailed “Active Conditions” summary document for signature (including credentials and date indication) for inclusion within the respective member’s medical record; (ii) clarified active condition and co-morbidity data (as may be used in coordination with encounter data for the purposes of risk score accuracy improvement); and (iii) further updated electronic medical record profile data maintained within ePASS for access and use by Authorized Users in the future as needed. |
| iv. | Encounter Documentation Review & Coding Validation: Upon the completion of each encounter, the Encounter Support ePASS platform shall convert each provider’s responses to a clinical encounter medical record note (known as an “Encounter SOAP Note”) consistent with CMS technical specification requirements and complete with electronic signature components of the utilizing provider (the “Completed ePASS Encounter SOAP Note”). |
| 1. | Encounter Document Review: Inovalon shall undertake a review of the Completed ePASS Encounter SOAP Note and confirm complete and accurate coding in a fashion that is compliant with CMS, or State Department of Health, as the case may be. |
| 2. | Encounter Document Provision & Copy: A copy of the Completed ePASS Encounter SOAP Note shall be made available to the utilizing provider (such copy may be in hard copy or electronic format depending on the utilizing provider’s request) and to Client in electronic format. |
| 3. | Encounter Document Risk Adjustment Coding: The clinical documentation coding (e.g., ICD) representative of each such Completed ePASS Encounter SOAP Note shall be converted into appropriate encounter format for the respective risk adjustment model reporting (e.g., RAPS File and EDS file format for CMS submission, or MEDS II File format for State Department of Health, as the case may be) and submission, if desired by Client. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 10 of 16
| v. | Provider Encounter Incentives: Client may choose to implement an incentive program for providers who utilize the ePASS platform completely. In the case, Inovalon shall include information of such incentive within the mailings and communication messages of the program to providers and will provide to Client on monthly basis information outlining provider participation so as to assist in the administration of such incentive programs. Such incentives, while strongly encouraged by Inovalon, shall be at the discretion of Client and paid at the expense of Client. |
| vi. | Provider Access to Member Information: Client’s Authorized Users (providers and support staff) can securely log into the ePASS platform via the Internet. Once such user’s credentials and password are authenticated, such users are able to access both historical information and a list of identified documentation, assessment, and care consideration gaps (and any associated Smart HRA question set, as the case may be) pertaining to such members (the group of such members being referred to as the “Provider Viewable Membership”). The Provider Viewable Membership additionally may be aggregated across a provider group with Client provision of such aggregation requirements. The Provider Viewable Membership is defined by a rule selected by Client as one of four options (indicated by a checkbox) below: |
| ☒ | Universal Member Loading – All providers identified by the Client as being Authorized Users can access all members for whom such provider has been identified as the Principally Relevant Member Provider; |
| ☐ |
Universal Gap Loading – All providers identified by the Client as being Authorized Users can access all members i) for whom such provider has been identified as the Principally Relevant Member Provider, and ii) for whom a Prospective Advantage Gap has been identified;
|
| ☐ |
Intervention Scheduled Loading – All providers identified by the Client as being Authorized Users can access all members i) for whom such provider has been identified as the Principally Relevant Member Provider, ii) for whom a Prospective Advantage Gap has been identified, and iii) for whom an intervention has been targeted; or
|
| ☐ |
Custom Loading – All providers identified by Client as being Authorized Users can access all members for whom such provider has been identified per a custom assignment list or algorithm (which will be mutually agreed to by Inovalon and Client).
|
| vii. | Notwithstanding any reductions in the Member Population during the term of the Agreement, Client’s Authorized Users (including providers) will be able to access and use the ePASS platform for all of Client’s Medicare Advantage members, including members that are not part of the Member Population. |
| c. | In-Home Assessment Processes. Inovalon shall identify members for whom Prospective Advantage Gaps are indicated, but for which an encounter with a provider is not, or has not, been able to be achieved (each a “Target Member”); thereafter coordinate and achieve an in-home provider assessment (or alternative assessment to the same end) and documentation; and provide such gained documentation, encounter coding, and associated information to the appropriate audiences and initiatives of Client to achieve improved clinical and quality outcomes, care management, and risk adjustment benefit for the respective Target Member, their primary care provider, and Client. So as to provide such service, Inovalon shall undertake the following: |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 11 of 16
| i. | Analytic Identification of Target Members: Inovalon will utilize analysis performed as outlined in this SOW, and additional algorithms within its PCIS and Identification, Stratification, and Prioritization (ISaP™) algorithms to identify and prioritize high-risk members (each referred to as a “Target Member”) who have: |
| 1. | Been identified as having Prospective Advantage Gaps; |
| 2. | Not responded to Encounter Facilitation Processes or Encounter Support Processes within three months of an outreach to achieve either or both of such; or |
| 3. | Been identified as having a high risk of negative clinical, quality, or financial impact in the absence of provider assessment (the determination rules of which shall be agreed to mutually by Inovalon and Client) and who have indicated an inability (or unwillingness) to achieve a provider encounter through traditional means (i.e., at an outpatient clinical office facility of a provider within Client’s provider network). |
| ii. | Member Outreach, Venue Selection, and Scheduling: Inovalon will outreach to each Target Member, determine best venue for the desired assessment (e.g., Target Member’s house, Target Member’s primary care provider’s outpatient clinical office, an Inovalon facility) for the achievement of the desired face-to-face provider assessment (the “Targeted Venue”), prepare the Target Member for the assessment process, and schedule a face-to-face assessment with the members. For the sake of clarity, for each Target Member, Inovalon seeks a prioritized approach to venue selection as follows: |
| 1. | Facilitate an encounter at the outpatient clinical office facility of the Target Member’s primary care provider by arranging appointment scheduling and coordinating transportation for Target Member; or |
| 2. | Facilitate an encounter at the Target Member’s house (or other location or facility, which may, for example, be a facility of Inovalon) by arranging appointment scheduling and coordinating transportation (as may be necessary) for Target Member. |
| iii. | Performance of Member Assessments: For those Target Members for whom an encounter with their primary care provider is unable to be facilitated, and for whom a face-to-face assessment has been able to be arranged, Inovalon’s subcontracted physicians or physician extenders, as defined by CMS technical specifications (the “Member Assessor”) will perform face-to-face, member assessments of such Target Members and document such member’s active disease and co-morbidities (the “Face-To-Face Member Assessment” and the documentation of such, the “Member Assessment SOAP Note”)). Prior to targeting an HMO member for a Face-To-Face Member Assessment, Inovalon will provide a list of potential targets to Client in writing for approval. Client will approve or reject such targets in writing within 10 business days of receipt of the list of potential targets. Once Client approves any potential target, Inovalon is deemed authorized to outreach to each such Target Member in accordance with this Section 6(c) and Client will not rescind such authorization unless requested by the Target Member. The Face-To-Face Member Assessments shall be guided by information and data known by Inovalon regarding such member, as enabled by Inovalon’s Electronic Patient Assessment Solution Suite (ePASS) and data-driven health risk assessment technology (SmartHRA), and shall include, with respect to the Target Member, the following as appropriate: |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 12 of 16
| 1. | Medical history (including chief complaint (CC), history of present illness (HPI), review of systems (ROS), past medical history (PMH), social history, family history and medications); |
| 2. | Physical exam (which shall generally include such segments as: general exam, eyes, ENT, neck, respiratory, cardiovascular, chest, abdominal, musculoskeletal, neurological, psychiatric, skin, and other such segments, as may change from time to time); |
| 3. | Diagnostics (as warranted and reasonably available, examples include pulse ox, ABIs, etc.); and |
| 4. | Assessment of current and chronic conditions. |
While the results of the Face-To-Face Member Assessment (i.e., the Member Assessment Encounter SOAP Note) are conveyed to Client and designated primary care provider, acknowledging that it is not the intention of the Face-To-Face Member Assessment to replace or supersede any primary care provider relationship, the Member Assessor shall render no management or treatment to the Target Member. The generality of the preceding sentence notwithstanding, in the event that the Member Assessor believes that the Target Member is in acute medical risk, the Member Assessor shall contact emergency services (e.g., 911) as warranted. For the sake of clarity the encounter shall not result in the delivery of treatment. Client shall be responsible for providing Inovalon with contact information for a liaison to support continuity of care for members receiving Face-To-Face Member Assessments.
Inovalon will conduct all Face-to-Face Member Assessments under the Agreement in a manner consistent with CMS “Guidance for In-Home Enrollee Risk Assessments” found on pages 144-146 of the 2016 Final Call Letter for Medicare Advantage plans or any updates or modifications of such guidance released by CMS from time to time. Inovalon and Client will work together to mutually agree on the “best practices” from the CMS guidance that are applicable to the Services. Additionally, Inovalon will actively monitor and audit its employees or contractors performing Face-to-Face Member Assessments to ensure that they are complying with all applicable provisions of such CMS guidance and the Agreement. Inovalon will provide detailed reports to Client of its monitoring and oversight activities of its employees and contractors performing Face-to-Face Member Assessments.
| iv. | Minimum Volume Commitments: As consideration for the reduced pricing for Face-To-Face Member Assessment Fees, Client hereby acknowledges and agrees that Inovalon will be permitted to target at least 90% of the members in Client’s PPO product line for Face-To-Face Member Assessments during each calendar year of the Term of this SOW. |
| v. | Quality Assurance Evaluation: Inovalon will evaluate and code each completed Assessment consistent with industry standard ICD and CMS/State Medicaid Agency technical specifications (the “Assessment Coding Data”). |
| vi. | Communication of Results: Inovalon will facilitate the provision of completed Assessments to the member’s designated primary care provider as designated by Client, and completed Assessments will be provided to Client in digital form on an encrypted DVD (or other secure media, as applicable). |
| vii. | Preparation of Diagnoses Submission Files: Inovalon will convert captured Assessment Coding Data into CMS-specific (and/or state-specific, in the case of Medicaid programs) encounter format for submission in advance of applicable regulatory deadlines. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 13 of 16
| d. | Supplemental Data for Specified Measures. Inovalon will convert from Completed ePASS Encounter SOAP Notes and from Member Assessment Encounter SOAP Notes data related to the measures listed below (the “Specified Measures”) which are able to be integrated into supplemental data stores for the purposes of quality score reporting as outlined by relevant regulatory or oversight bodies (e.g., as outlined within NCQA guidelines as listed within Volume II Technical Specifications, and any such similar materials of CMS) as applicable. Such supplemental data will be exchanged by and between the parties in Inovalon’s Pseudoclaim™ format (each a “Pseudoclaim” and the format, the “Pseudoclaim Format”) as outlined within Inovalon’s then current Pseudoclaim Import-Export Specifications document. Any time required to undertake any additional conversions will be considered Support Units as outlined under Section 10. For the sake of clarity, Pseudoclaims and the associated technical specifications of such Pseudoclaim Format are proprietary to Inovalon and are Inovalon Intellectual property, not to be shared with any other party. For purposes of this SOW, the Specified Measures are: |
| i. | Adult BMI assessment; |
| ii. | Care for older adults – medication review; |
| iii. | Care for older adults – functional status assessment; |
| iv. | Care for older adults – pain screening; |
| 7. | Service Level Agreements (SLAs). |
| a. | Member Assessment SOAP Note processing timing. For each Member Assessment SOAP Note received by Inovalon in completed form without errors or omissions inhibiting processing by Inovalon as outlined within this SOW, Inovalon agrees to review, code and process each such valid Member Assessment SOAP Note within ten (10) business days for electronic Member Assessment SOAP Notes received through ePASS. |
| i. | Method of Determination of SLA Performance. This SLA will be measured on a monthly basis. |
| ii. | Consequences of Failure to Meet SLA. Inovalon will be penalized ten percent (10%) of the Encounter Support Fee for each Member Assessment SOAP Note that fails to meet this SLA. |
| b. | ePASS Enhancement & Change Notification. Inovalon will provide 30 days’ advance notice to Client of any user interface and content changes (including but not limited to any changes made to comply with regulatory requirements) to ePASS so that Client may share this information with Authorized Users. In such cases related to regulatory compliance where the regulator provides Inovalon less than 30 days to notify the changes, Inovalon will notify Client as soon as reasonably possible within the timeframe provided by the regulatory agency. In cases of emergency changes related to software performance and security, Inovalon will provide notice to Client of the change as soon as reasonably possible but no later than (2) two business days after the change is made. |
| i. | Consequences of Failure to Meet SLA for Changes to ePASS. If Inovalon fails to provide notice to Client within the timeframes described in previous sub-section 7 (b) and the resulting changes impact Client, Inovalon will issue a credit to the second party equal to $5,000 per SLA violation. |
| 8. | Reporting. To the extent applicable to the Services hereunder, Inovalon shall provide the following reports: |
| a. | Encounter Impact Tracking and Reporting: Inovalon shall provide process impact reporting to Client as follows: |
| i. | Encounter Tracking: Inovalon shall track the number and claims’ disease condition coding of encounters achieved through the activities of this SOW. The results of such tracking shall be provided to Client within a report (referred to as an “Encounter Impact Report”). |
| ii. | Disease Related Utilization Tracking: Inovalon shall track utilization preceding and following encounters achieved through the activities of this SOW. The results of such tracking shall be provided to Client within a report (referred to as a “Utilization Impact Report”). |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 14 of 16
| iii. | Risk Adjustment Impact Tracking: Inovalon shall track the financial result of risk adjustment factor improvements following encounters achieved through the activities of this SOW. The results of such tracking shall be provided to Client within a report (referred to as a “Factor Impact Report”). |
| iv. | Summary Impact Tracking: Inovalon shall provide a summary impact report outlining the combined impact of utilization and risk score accuracy achieved through the activities of this SOW. The results of such shall be provided to Client within a report (referred to as a “Summary Impact Report”). |
| b. | Encounter Support Impact Tracking and Reporting: So as to enable Client’s measurement and monitoring of the Encounter Support performance, as well as to provide results transparency and progress tracking capabilities, Inovalon shall make available to Client access to the reports noted below. The reports will be available to Client through the Client Web Portal. Such reports include (as may be periodically revised, modified, supplemented, and expanded): |
| i. | Provider ePASS Portal utilization reports; |
| ii. | Member encounter activity reports; |
| iii. | Documentation Gap closure reports; |
| iv. | Assessment Gap closure reports; |
| v. | Care Consideration Gap closure reports; and |
| vi. | Realized financial impact reports. |
REIMBURSEMENT AND PAYMENT SCHEDULE FOR SERVICES
| 9. | Fees and Expenses. For the services outlined within this SOW, Inovalon will charge and invoice Client as follows: |
| a. | Process Analytics & Reporting Fees: Beginning on the SOW Effective Date Inovalon will charge a monthly base processing fee equal to the Prospective Advantage Processing Fee plus the Specific Measures Processing Fee (the “Base Processing Fee”) for the Member Population as noted in Table 1 below and a total member count related fee (the “PMPM Processing Fee”) as outlined within the Table 1 below. The sum of the Base Processing Fee and PMPM Processing Fee shall be invoiced monthly in arrears (prorated for partial months). The fees shall be based on the Member Population(s) from the most recently received Health Plan Data Set (and the member counts provided in Table 1 in the absence of any Health Plan Data Set). |
|
Member Population
|
Population
Members
Enrolled
|
Prospective
Advantage
Processing Fee
|
Specific Measures
Processing Fee
|
PMPM Processing
Fee
|
|
Triple-S Advantage Inc. (H4005)
|
121,743
|
$ 19,575
|
$ 4,950
|
$ 1.63
|
Table 1: Prospective Advantage Monthly Processing Fees
| b. | Gap Resolution Fees: Inovalon shall charge a fee for the performance of gap resolution activities on a monthly basis in arrears as outlined below: |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 15 of 16
| i. | Encounter Facilitation Fee: For each Encounter Facilitation, Inovalon will charge Client a fee of $27.71 (the “Encounter Facilitation Fee”). |
| ii. | Encounter Support Fees: For each Encounter Support, Inovalon will charge Client a fee of $47.00 (the “Encounter Support Fee”) plus an additional fee of $3.96 (the “Specified Measures Fee”) for the conversion and processing related to the Specified Measures. Inovalon will charge $20.18 plus the Specified Measures Fee for any Converted Encounter Facilitation. |
| iii. | Face-To-Face Gap Member Assessment & Closure Fees: Inovalon shall charge Client a fee of $268.64 (the “Face-To-Face Member Assessment Fee”) for each Face-To-Face Member Assessment performed plus the Specified Measures Fee for the conversion and processing related to the Specified Measures, plus the cost of mileage according to IRS mileage reimbursement rates (the “Mileage Reimbursement Fee”). |
| c. | Pass-Through Fees: Inovalon will charge to Health Plan the cost for the pass-through items outlined below, at cost, each of which shall be outlined in reasonable detail by Inovalon (the “Pass-Through Fees”). |
| i. | Hardcopy fulfillment of member and provider notification letters (sent via USPS and FedEx, as the case may be), and the fulfillment expenses therefore (together, referred to as the “Hardcopy Fulfillment Expense Pass-Through”); |
| ii. | The cost of any incentives offered to Client’s providers and/or members upon completion of an intervention and all administration and mailing costs associated with any such incentives offered; and |
| iii. | Mileage driven on behalf of the performance of services under this SOW will be reported and charged at the IRS Mileage Reimbursement Fee for each such mile (the “Mileage Pass-Through”). |
| 10. | Provision of Support Services. Client may, in its sole discretion, utilize support units (“Support Units”) in any proportion for the provision by Inovalon of support services outside the scope the Services. Inovalon will invoice Client for the Support Units in arrears at the price of $50 per Support Unit. Client may elect to use the Support Units for Client IT / Prospective Advantage integration support and/or client operations process improvement consulting services and Inovalon agrees to provide to Client IT / Prospective Advantage integration support and/or client operations process improvement consulting services (“Support Services”). In the event that a Client request for Support Services is expected to incur Support Units, Inovalon will provide a good faith estimate to Client and receive Client’s written approval prior to beginning such work related to such request for Support Services. |
| a. | Support Units are determined based on the following levels of support. |
| i. | Level 1 Support: Support questions regarding basic technical questions which are not product specific (e.g. questions regarding logging into the Inovalon Client Web Portal. An example of Level 1 Support (which is always included) is technical assistance in accessing ePASS or the Client Web Portal. |
| ii. | Level 2 Support: Support questions which are product-specific (i.e. specific to the Prospective Advantage solution, services, and/or subject matter) and which are considered basic in their complexity as well as product-specific training. An example of Level 2 Support (which is always included) is the daily operational support of the client services organization including reviewing the Prospective Advantage Financial Impact Report, or product specific training such as CARA issues log training. |
Master Services Agreement
Statement of Work #1 - Prospective Advantage®
Page 16 of 16
| iii. | Level 3 Support: Support questions which are product-specific (i.e. specific to the Prospective Advantage solution, services, and/or subject matter) and which are considered advanced in their complexity, but which do not require a senior management person’s involvement (i.e. not requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 3 Support is generating a specific financial report investigating particular HCC’s or medical conditions by a particular medical group. |
| iv. | Level 4 Support: Support questions which are product-specific (i.e. specific to the Prospective Advantage solution, services, and/or subject matter) and which are considered highly advanced in their complexity, therefore requiring (or, at the request of the Client, involving) involvement of a product leader, Senior Director (or higher), or Medical Director). An example of Level 4 Support is performing a risk adjustment accuracy project which compares found HCC’s by a specific medical group on a year over year basis. |
| b. | Support Units are calculated based on the amount of time and the level of support utilized as set forth in Table 2 below. |
|
Support Level
|
Number of Units /
Hour
|
Cost by the Hour*
|
|
Level 1
|
Included within scope of Services
|
|
|
Level 2
|
Included within scope of Services
|
|
|
Xxxxx 0
|
0
|
x 000
|
|
Xxxxx 4
|
6
|
$ 300
|
Table 2: Support Units
* Level 3 and Level 4 are calculated in hourly increments.
| 11. | .General Invoicing. Except as otherwise provided above, Inovalon will invoice Client for the Services provided on a monthly basis in arrears. |
| 12. | Specification Changes. In the event that CMS or State Department of Health should materially change the risk adjustment reimbursement technical specifications, Inovalon reserves the right to adjust the fee structure outlined within this SOW accordingly; provided, however, that such fee structure changes, if any, must be reasonable, proportional to the changes in such technical specifications. |
| 13. | Limitations of Data Accuracy. Both parties acknowledge that the accuracy and completeness of the Services may be limited by inaccuracies and incompleteness, if any, within data provided by Client to Inovalon. |
Master Services Agreement
Statement of Work #2 – INDICES™ Business Intelligence
Page 1 of 5
Statement of Work #2
INDICES™ BUSINESS INTELLIGENCE (“BI”) REPORTING PLATFORM
SCOPE OF SERVICES
This Statement of Work #2 (this “SOW”) is entered into and effective as of the Effective Date (the “SOW Effective Date”) of that certain Master Services Agreement effective January 1, 2016 (as amended, the “Agreement”) by and between Inovalon, Inc. and Client pursuant to the terms and conditions thereof. Inovalon will use all commercially reasonable efforts to provide the following BI reporting services (the “Services”) in a professional and workmanlike manner.
| 1. | Overview of Scope. Inovalon shall provide an online, web-enabled reporting platform (referred to as the “Business Intelligence Reporting Platform” or “BI Reporting Platform”) to enable Client access to relevant managed care information regarding its members, providers, and facilities in areas of, amongst others, demographic information, clinical and quality outcome information, cost and utilization information, revenue and risk adjustment information, and clinical program information. |
| 2. | Term and Termination. This SOW shall commence on the Effective Date and shall continue in effect through December 31, 2017 |
| a. | Transition Services. In the event of termination or expiration of the Agreement, Inovalon will provide the support described below up until the end of the Transition Period (as defined below) both (A) in accordance with all standards set forth in the Agreement and this SOW and (B) with the same level of accuracy, intensity and timeliness of Services performed before receipt of the notice of termination or non-renewal, meeting all the data specifications required by Client and CMS. In consideration of the transition services, Inovalon will continue to invoice and Client will continue to pay the Base Processing Fee described in Section 6 of the SOW during the 3 month period following the Termination Date (the “Transition Period”). |
| i. | Inovalon will make available through the INDICES Platform all analytics performed up until the Termination Date; and |
| ii. | Inovalon will keep available and accessible the INDICES Platform until the end of the Transition Period |
| 3. | Reporting Domain Content. The INDICES BI Reporting Platform shall provide access to information domains as outlined within Schedule 1 of this SOW (the “Information Domain Components”). |
| 4. | Timelines. The provision of the Information Domains within the BI Reporting Platform shall be undertaken in accordance to a timeline described within Schedule 1 of this SOW. Each domain category shall be made available within the BI Reporting Platform on or before the last calendar day of the month indicated as the respective domain’s “Initial Implementation Date.” The period immediately following each Initial Implementation Date shall be considered a period for testing and review by both Client and Inovalon (the “Review & Testing Period”). Such period is anticipated to require up to 3 months. Following the completion of the Review & Testing Period, one or more updates to the BI Reporting Platform shall implement any necessary changes and the initial release of such domain category shall be deemed complete (the date on which such is achieved being referred to as the “Service Pack 1 Release Date” for such respective domain). |
Master Services Agreement
Statement of Work #2 – INDICES™ Business Intelligence
Page 2 of 5
| 5. | Access Rights. Client shall have full access to all Medical Records, ePASS and Face-To-Face Member Assessments completed as described in SOW #1 (Prospective Advantage), and SOW #4 (CARA). Additionally, Client will have access through the BI Reporting Platform to all available portals and reporting, among others services included herein without any user amount limit. |
| 6. | Fees. Beginning on the SOW Effective Date, Inovalon will charge a monthly base processing fee (the “Base Processing Fee”) as outlined within Table 1 below and a total member count related fee (the “PMPM Processing Fee”) calculated by multiplying the number of members within each Reporting Population by the “Monthly PMPM Processing Fee” as outlined within the table below. The sum of the Base Processing Fee and PMPM Processing Fee shall be invoiced monthly in arrears. |
|
Reporting Population
|
Population
Members
Enrolled
|
Base
Processing
Fee
|
Monthly
PMPM
Processing
Fee
|
|
Triple-S Advantage, Inc.(H4005)
|
121,743
|
$ 1,3495.19
|
$ 0.125
|
Table 1: BI Reporting Platform Monthly Processing Fees
| 7. | Provision of Support Services. Client may, in its sole discretion, utilize support units (“Support Units”) in any proportion for the provision by Inovalon of support services outside the scope the Services. Inovalon will invoice Client for the Support Units in arrears at the price of $50 per Support Unit. Client may elect to use the Support Units for Client IT / BI integration support and/or client operations process improvement consulting services and Inovalon agrees to provide to Client IT / BI integration support and/or client operations process improvement consulting services (“Support Services”). In the event that a Client request for Support Services is expected to incur Support Units, Inovalon will provide a good faith estimate to Client and receive Client’s written approval prior to beginning such work related to such request for Support Services. |
| a. | Support Units are determined based on the following levels of support. |
| i. | Level 1 Support: Support questions regarding basic technical questions which are not product specific (e.g. questions regarding logging into the Inovalon Client Web Portal). An example of Level 1 Support (which is always included) is technical assistance in accessing ePASS or the Client Web Portal. |
| ii. | Level 2 Support: Support questions which are product-specific (i.e. specific to BI Reporting Platform, services, and/or subject matter) and which are considered basic in their complexity as well as product-specific training. An example of Level 2 Support (which is always included) is the daily operational support of the client services organization including reviewing the Prospective Advantage Financial Impact Report, or product specific training such as CARA issues log training. |
| iii. | Level 3 Support: Support questions which are product-specific (i.e. specific to the BI Reporting Platform, services, and/or subject matter) and which are considered advanced in their complexity, but which do not require a senior management person’s involvement (i.e. not requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 3 Support is generating a specific financial report investigating particular HCC’s or medical conditions by a particular medical group. |
Master Services Agreement
Statement of Work #2 – INDICES™ Business Intelligence
Page 3 of 5
| iv. | Level 4 Support: Support questions which are product-specific (i.e. specific to the BI Reporting Platform solution, services, and/or subject matter) and which are consider highly advanced in their complexity, therefore requiring (or, at the request of the Client, involving) a senior management person’s involvement (i.e. requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 4 Support is performing a risk adjustment accuracy project which compares found HCC’s by a specific medical group on a year over year basis. |
| b. | Support Units are calculated based on the amount of time and the level of support utilized as set forth in Table 2 below: |
|
Support Level
|
Number of Units /
Hour
|
Cost by the Hour*
|
|
Level 1
|
Included within scope of Services
|
|
|
Level 2
|
Included within scope of Services
|
|
|
Xxxxx 0
|
0
|
x 000
|
|
Xxxxx 4
|
6
|
$ 300
|
Table 2: Support Units
* Level 3 and Level 4 are calculated in hourly increments.
| 8. | Limitations of Data Accuracy. Both parties acknowledge that the accuracy and completeness of the Services provided within this SOW may be limited by inaccuracies and incompleteness, if any, within data provided by Client to Inovalon. |
| 9. | Platform Access. Inovalon will undertake commercially reasonable efforts to ensure the INDICES Platform availability for 99.9% of the time during each calendar month. Any changes to the INDICES Platform will be made with reasonable previous notification to Client. |
| a. | “System Availability" means the percentage of total time during which the INDICES Platform is available to Client, excluding the Scheduled Maintenance Period, Emergency Maintenance or force majeure events. All scheduled maintenance period and emergency maintenance will be made with reasonable previous notification to Client. |
| b. | In the event that the INDICES Platform does not meet the monthly service availability defined herein, Inovalon will provide a credit against the monthly invoice under this SOW to the Client in accordance to the table below. |
|
Percent of INDICES Platform
Availability per Calendar Month
|
Service Credit
|
|
<99.9%
|
2%
|
|
<99.0%
|
5%
|
|
<98.0% (being 3 days)
|
10%
|
Table 3: Service Credits
Master Services Agreement
Statement of Work #2 – INDICES™ Business Intelligence
Page 4 of 5
| c. | When possible, Inovalon will notify Client within a reasonable time of any Service Outage. Client will register a log of any outage incidents which will be shared with Inovalon for credit claims purposes. This outage incident log will document the date and the amount of time when Client experiences a disruption in availability of the INDICES Platform. For determining the Credit, the duration of a Service Outage will be measured as the time starting when Client experiences a disruption in availability of the INDICES Platform and ending when a successful solution or workaround allowing for full restoration of the INDICES Platform is provided by Inovalon to Client. |
| d. | Any Credits earned by Client hereunder will be applied to the Monthly Based Processing Fees owed by Client for the next month for which the Credit applies. If Credits cannot be applied to future Fees because the Agreement has terminated (or due to a material uncured breach by Inovalon which caused the Agreement to terminate), Inovalon will pay Client the amount of the Credit. |
Master Services Agreement
Statement of Work #2 – INDICES™ Business Intelligence
Page 5 of 5
Schedule 1 to Statement of Work #2
INDICES BI Reporting Platform Domain Content Schedule
|
Domain Area
|
Domain Name
|
Domain Components
|
Domain
Implementation Time
|
|
1
|
Membership
(Member / Enrollment
Analysis & Reporting
|
● Member Details (Key demographics, Plan information and Contact information)
● Plan membership analyses including by Age & Gender, Payer and Product, Density by County
● Longitudinal membership trending including the Turnover Trend Analysis
|
Upon the SOW
Effective Date
|
|
2
|
Member and Provider Search
(Member, PCP and PCP Group Profiles)
|
● Member Cross-Product and Cost/Utilization Profile
● Provider (PCP) and Provider Group Cost/Utilization Panel Profile and Roster Analysis
● Provider / Group Longitudinal Comparison across key metrics
|
Upon the SOW
Effective Date
|
|
3
|
Pharmacy & Medical
(Cost & Utilization Analysis and Reporting)
|
● Medical Cost & Utilization Trending (Inpatient, Outpatient & Ancillary Services)
● Medical Utilization by Provider Specialty, by Region, by plan group, by age/gender/geography
● Medical Utilization Admits/Visits per 1000 Trending
● Pharmacy Cost & Utilization trends/comparisons by NDC Categories, Diagnosis categories, brand/generic drug types, provider specialty, by plan group, by age/gender/geography
● Pharmacy Drug Top 10 Analysis (HRM, Brand vs Generic, and Maintenance Drugs)
|
Upon the SOW
Effective Date
|
|
5
|
Risk Adjustment
(Risk Adjustment membership analysis, Retrospective Risk Adjustment Analysis and Reporting and Prospective Risk Adjustment Analysis and reporting)
|
Medicare MMR/MOR Reporting:
● Member risk score trends, Plan payment adjustments, Member Original Reason for Entitlement, Member Status (Hospice, ESRD, and Medicaid), Member Benefit Indication (Part A, B, D) and Member Factor Type (Community, Institutional, ESRD) , Membership by Acute/Chronic condition
CARA®
● Member Retrospective Outreach Activity (Provider Reviewed by Month & Year)
● Member Retrospective Outreach CEDIs by CEDI Process
● Member HCC Realization Analysis and Improvement Reporting
Prospective Advantage®
● Member Outreach Activity (Interventions by Month & Year)
● Member HCC Realization and gap closure analysis and Improvement Reporting
|
Upon the SOW
Effective Date
|
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 1 of 7
Statement of Work #3
MEDICARE ADVANTAGE
CLAIMS AGGREGATION, ANALYSIS, AND SUBMISSION (CAAS™)
SOLUTION SERVICES
This Statement of Work #3 (this “SOW”) is entered into and effective as of January 1, 2016 (the “SOW Effective Date”) pursuant to the terms and conditions of that certain Master Services Agreement effective January 1, 2016 (the “Agreement”) by and between Inovalon, Inc. (“Inovalon”) and Triple-S Advantage, Inc., (“TSA”), administered by Triple- S Advantage Solutions, Inc. (“Client”). Inovalon will use all commercially reasonable efforts to provide the following CAAS services (the “Services”) in a professional and workmanlike manner.
| 1. | Term and Termination. This SOW shall commence on the SOW Effective Date and shall continue in effect through December 31, 2017 (the “Term”). |
| a. | It is acknowledged that CMS is proposing a change to file submission format. The proposed format (the “EDS Format”) will be a separate and distinct filing from the current format (the “RAPS Format”) and both formats (RAPS and EDS) are expected to be necessarily submitted to CMS in parallel for some period of time (a period which is expected to be one to three years). Notwithstanding anything set forth in this SOW or the Agreement, this SOW may terminate at Client’s request in the event that RAPS Files (defined below) are no longer accepted by CMS. |
| b. | Transition Services. In the event of termination or expiration of the Agreement, Inovalon will provide the following support up until the end of the Transition Period (as defined below) both (A) in accordance with all standards set forth in the Agreement and this SOW and (B) with the same level of accuracy, intensity and timeliness of Services performed before receipt of the notice of termination or non-renewal, meeting all the data specifications required by Client and CMS. |
| i. | Inovalon will perform all analytics described in this SOW up until the Termination Date, meeting all the data specifications required by Client and CMS; and |
| ii. | Inovalon will make available the results of all analytics performed up until the Termination Date during the 3 month period following the Termination Date (the “Transition Period”). |
| 2. | Authorization; CMS System Requirements. |
| a. | Client currently submits its own data to CMS. Should Client elect at a later date to have Inovalon serve as a CMS third-party Risk Adjustment Data Submitter on its behalf: |
| i. | Client shall appoint Inovalon to serve as its third party submitter for the submission of Client’s Medicare risk adjustment data in respect to each Medicare Advantage Member Population (each, a “RAPS Member Population”) set forth in Table 1 below. Client acknowledges and understands, that pursuant to CMS requirements, regardless of who submits the Medicare risk adjustment data, CMS holds Client accountable for the content of the data; |
| ii. | Client’s election (if made) shall be made by completion of all applicable CMS Electronic Data Interchange Enrollment Forms (“EDI Arrangements”), which Client will maintain current, and shall provide Inovalon with copies thereof (including all amendments or other modifications thereto). Client shall thereafter provide prompt notice to Inovalon of any termination of such EDI Arrangements with CMS; and |
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 2 of 7
| iii. | Client shall further provide Inovalon with the information required on the attached Data Sheet and such other information reasonably requested by Inovalon in connection with the services contemplated hereunder. Client shall thereafter promptly notify Inovalon in the event of any material changes to such information. |
| b. | Inovalon shall generate and provide to Client a Risk Adjustment Processing System (RAPS) file (a “RAPS File”) in respect to resulting claims data for review by Client and submission, in whole or in part at the sole discretion of the Client, to CMS. Client hereby elects for Inovalon to provide RAPS Files to Client on a monthly basis. Inovalon will submit RAPS files to Client in the latest International Classification of Diseases Edition as required by CMS. At the Agreement Effective Date Inovalon will submit to Client its ICD-10 readiness plan. Non-compliance with this ICD requisite will result in a penalty (to be credited to Client) of five percent (5%) of the monthly fees paid to Inovalon for each month in which Inovalon fails to comply with this CMS requirement, in addition to and not in lieu of other remedies available under the Agreement (except other SLA Penalties). If Inovalon fails to comply with this CMS requirement, it will be considered a material breach of the SOW subject to termination in accordance with Section 3.2(b) of the Agreement. Additionally, if as a result of an error or omission made by Inovalon to comply with this requirement, CMS imposes a penalty on or assesses interest against Client, Inovalon will pay to Client all penalties directly attributed to Inovalon’s error or omission, subject to any limitation of liability described in the Agreement. This section shall survive termination of the Agreement or any SOW. |
| 3. | Data Transfer and Transform Processing; Client Data Repository. |
| a. | Inovalon shall work with designated Client personnel in the provision of a secure and complete transfer of Member Population data (each a “Health Plan Data Set”) between Client data to Inovalon via secure FTP portal using established transfer, compression, and encryption protocols. For ongoing RAPS File production, Inovalon shall established a transfer schedule for core data components (occurring monthly) in order to allow for the timely production of RAPS Files and reporting. |
| i. | Specification of Health Plan Data Set: Inovalon will provide Client with a comprehensive outline of data required by Inovalon for the data processing of each Member Population (which will constitute components of the Health Plan Data Set for each such Member Population) including, amongst other data, the: |
| 1. | Member demographics data; |
| 2. | Member claims and cost data; |
| 3. | Member enrollment data; |
| 4. | Member laboratory data; |
| 5. | Member pharmacy data; |
| 6. | Member durable medical equipment data; |
| 7. | Care provider data; |
| 8. | MOR detail data; and |
| 9. | MMR detail data. |
| b. | All data received from Client shall be staged in its raw formats in order to allow for full source file attribution, audit trailing, and mapping reconciliations. Client must notify Inovalon of any change to Client’s raw formats so as to facilitate accurate and efficient integration into the Client Data Repository (CDR). |
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 3 of 7
| c. | All data translations, crosswalks and mapping into the CDR shall be performed by Inovalon data analyst staff. As data is mapped into the CDR, data fields will be evaluated for consistency with expected values. All files imported into the CDR shall be tracked, tagged, and indexed, to allow for efficient processing and attribution of results to imported data files. Further, member and provider matching rates will be analyzed for encounter files and third-party claims and Inovalon shall work with designated Client personnel to resolve data consistency, data gaps, and data value validation issues and to facilitate appropriate data source matching and reconciliation. |
| d. | Inovalon and Client shall jointly review, validate, and approve the translations, crosswalks, and mapping protocols of raw data to facilitate the accurate loading and maintenance of the CDR. |
| 4. | RAPS File Processing. |
| a. | Inovalon shall work with designated Client personnel to identify and integrate all available sources of member and diagnosis data to validate that all relevant data has been obtained and utilized, and that the data that has been provided is comprehensive. This process is achieved through a systematic and structured approach, utilizing extensive logging and tracking of data, evaluation of prevalence trends in membership, enrollments, and claims, data densities for encounters, prescription drugs, and laboratory results, and exception tracking for enrolled members without care provision events. |
| b. | Upon completing the integration and validation of included data files and configuration of Inovalon’s systems to accommodate Client specific characteristics, Inovalon shall perform an HCC Model Run, based upon the methodology for calculating members’ risk factors as prescribed by CMS, including: |
| i. | Identification of diagnoses that relate to HCCs; |
| ii. | Cross-reference of diagnosing practitioner against “valid” practitioner listing and NPI Registry; |
| iii. | Evaluation of data for Age/Sex edits; |
| iv. | Grouping of diagnoses into HCC hierarchical categories to attribute “highest value” HCC, and elimination of duplicate HCC diagnoses for submission; and |
| v. | Identification of Demographic and Disease Interactions for duel eligible members having certain HCC incidents and co-morbidities |
| c. | Inovalon shall prepare all of Client’s Medicare risk adjustment data for the Member Population in CMS-specified RAPS Format and provide to Client for processing and submissions. Inovalon shall process such claims data provided by Client so as to conform with RAPS Format specifications. When producing each RAPS File, Inovalon will perform a “differential” analysis against previously submitted RAPS Files to minimize the risk that duplicate submissions will occur. It is understood, however that certain errors cannot be checked or validated by Inovalon alone, including errors related to member enrollment and provider validity within CMS records and other related issues outside of Inovalon’s control, and as such, Inovalon shall not be responsible for resolving any such errors. |
| d. | Inovalon shall utilize the Health Plan Data Set received from Client on or before the 10th of a specific month (the “Monthly Processing Period”) for the production of the month’s RAPS File, which shall be completed and made available to Client (and submitted to CMS , as the case may be) by the end of the same month. For the sake of example, data provided by Client to Inovalon on or before February 10th, shall be utilized in the production of the RAPS File that is to be available and provided to Client (and CMS, as the case may be) by the last day of February, and the month of February is referred to as the Monthly Processing Period. |
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 4 of 7
| e. | In the event that Client elects to utilize Inovalon as its submitter to CMS as outlined under 2(a), Inovalon shall provide a copy of each RAPS return file (each, a “RAPS Return”) and CMS submission reconciliation report (each, a “CMS Reconciliation Report”) to Client. It shall be the responsibility of Client to make any appropriate corrections to its claims data, membership data, member enrollment data, or other relevant data source in response to errors identified on the CMS Reconciliation Reports. Any changes or corrections received by Inovalon from Client will be processed for the next applicable subsequent submission. |
| f. | Client may elect to provide weekly Health Plan Data Sets to Inovalon. In the event Client elects to provide weekly Health Plan Data Sets and requests that Inovalon process weekly RAPS Files, Inovalon will process weekly RAPS Files and will invoice Client $0.10 per Actual Enrolled Member (in addition to the Monthly RAPS File Production Fee) for each weekly RAPS File production process performed above the once monthly process. |
| g. | Client will provide monthly files containing HCC codes to be incorporated into RAPS files by Inovalon (“Special Files”). The Special Files will be provided to Inovalon by a day of the month mutually agreed upon by the parties. Inovalon agrees to process the Special Files through its de-duplication logic and add the data they contain to Client’s RAPS files at no additional charge to Client. |
| 5. | Reporting and Analytics. Inovalon shall provide reporting and project management capabilities, which shall all be available through the Client Web Portal, including reporting and analytical tools, which span from project management through financial impact assessment, vendor performance, and network practitioner performance improvement. |
| 6. | Resources. Inovalon shall allocate the resources necessary with respect to the hardware, software, and personnel for the receipt, integration, storage, maintenance, processing, and reporting of Client data and resulting RAPS Files and associated reporting. Such resources shall be allocated regardless of Client’s provision of data. As such, Client acknowledges that it is the responsibility of Client to provide the necessary data outlined under this SOW and that the absence of such provision or any other Client responsibility hereunder does not result in the avoidance of any of the monthly fees outlined under this SOW, specifically the CDR Monthly Maintenance Fee, Monthly RAPS File Production Fee, and (if applicable) Monthly RAPS File Submission Fee (together, the “Monthly Fees”). In the event that the calculation of such Monthly Fees is compromised by the absence or incomplete provision of data or support by Client, then such month’s Monthly Fees shall be the greater of those which are able to be calculated or the prior months invoiced Monthly Fees. |
| 7. | Service Level Agreements (SLAs). |
| a. | File Process Timing. Inovalon will: (A) make available to Client RAPS within 1 business day of the mutually agreed upon delivery date; and (B) provided that Client continues to share the Daily Membership Intake File in the current format (or other mutually agreed upon format), process the Daily Membership Intake File within 3 business days of receipt. |
| i. | Method of Determination of SLA Performance. This SLA will be measured on a monthly basis. |
| ii. | Consequences of Failure to Meet SLA. If Inovalon is out of compliance with either of the timelines above for three days or more, Inovalon will provide a Corrective Action Plan and will be penalized ten percent (10%) of the CDR Monthly Maintenance Fee for the applicable month. |
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 5 of 7
| 8. | Pricing. |
| a. | Client Data Repository Maintenance & Monthly Base Processing Fee. Beginning on the SOW Effective Date, Inovalon will charge a monthly fee equal to $5,101.18(the “CDR Monthly Maintenance Fee”) for the Member Population as noted in Table 1 below for the maintenance of the CDR and the ongoing import, validation, mapping, and cross-walking of client data into the CDR. This fee includes the integration and maintenance of data from Client and Inovalon. Should additional data sources be utilized in the CDR, the monthly fee shall be increased by $1,725 per additional data source (the “Monthly Additional Data Source Fee”, with a one-time integration, validation, and mapping fee of $12,250). |
| b. | Monthly RAPS File Production, Reconciliation, & Reporting. Beginning on the SOW Effective Date, Inovalon will charge a fee for the monthly production of RAPS Files from Client’s practitioner data, encounters, claims, and third party diagnoses, with appropriate reconciliation and reporting as described in this SOW, identified as the “Monthly RAPS File Production Fee” in Table 1 below for each member enrolled in Client’s health plan(s) (or additional Member Populations or such sub-populations unless otherwise agreed to mutually) as indicated within the data processed for such Monthly Processing Period (an “Actual Enrolled Member”). |
|
Member Population
|
Expected
Enrolled
Member
Count
|
Monthly RAPS
File Production
Fee (per Actual
Enrolled Member)
|
|
Triple-S Advantage, Inc. (H4005)
|
121,743
|
$ 0.48*
|
Table 1: Monthly Processing Fees
*in accordance with Section 4(f) of this SOW an additional $0.10 PMPM may be assessed should Client elect more frequent production
| c. | Monthly RAPS File Processing & Submission Fee. In the event Client chooses to have Inovalon serve as its CMS third-party Risk Adjustment Data Submitter as outlined under Section 2(a), for processing, formatting, and submission of Client’s Medicare risk adjustment data, Inovalon shall charge Client a monthly fee (the “Monthly RAPS File Submission Fee”) equal to $5,700. |
| 9. | Provision of Support Services. Client may, in its sole discretion, utilize support units (“Support Units”) in any proportion for the provision by Inovalon of support services outside the scope the Services. Inovalon will invoice Client for the Support Units in arrears at the price of $50 per Support Unit. Client may elect to use the Support Units for Client IT / CAAS integration support and/or client operations process improvement consulting services and Inovalon agrees to provide to Client IT / CAAS integration support and/or client operations process improvement consulting services (“Support Services”). In the event that a Client request for Support Services is expected to incur Support Units, Inovalon will provide a good faith estimate to Client and receive Client’s written approval prior to beginning such work related to such request for Support Services |
| a. | Support Units are determined based on the following levels of support. |
| i. | Level 1 Support: Support questions regarding basic technical questions which are not product specific (e.g. questions regarding logging into the Inovalon Client Web Portal). An example of Level 1 Support (which is always included) is technical assistance in accessing ePASS or the Client Web Portal. |
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 6 of 7
| ii. | Level 2 Support: Support questions which are product-specific (i.e. specific to the Prospective Advantage solution, services, and/or subject matter) and which are considered basic in their complexity as well as product-specific training. An example of Level 2 Support (which is always included) is the daily operational support of the client services organization including reviewing the Prospective Advantage Financial Impact Report, or product specific training such as CARA issues log training. |
| iii. | Level 3 Support: Support questions which are product-specific (i.e. specific to the CAAS solution, services, and/or subject matter) and which are considered advanced in their complexity, but which do not require a senior management person’s involvement (i.e. not requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 3 Support is generating a specific financial report investigating particular HCC’s or medical conditions by a particular medical group. |
| iv. | Level 4 Support: Support questions which are product-specific (i.e. specific to the CAAS solution, services, and/or subject matter) and which are consider highly advanced in their complexity, therefore requiring (or, at the request of the Client, involving) a senior management person’s involvement (i.e. not requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 4 Support is performing a risk adjustment accuracy project which compares found HCC’s by a specific medical group on a year over year basis. |
| b. | Support Units are calculated based on the amount of time and the level of support utilized as set forth in Table 2 below. |
|
Support Level
|
Number of Units /
Hour
|
Cost by the Hour*
|
|
Level 1
|
Included within scope of Services
|
|
|
Level 2
|
Included within scope of Services
|
|
|
Xxxxx 0
|
0
|
x 000
|
|
Xxxxx 4
|
6
|
$ 300
|
Table 2: Support Units
* Level 3 and Level 4 are calculated in hourly increments.
| 10. | Specification Changes. In the event that CMS should materially change the HCC technical specifications or RAPS file technical specifications Inovalon reserves the right to adjust the fee structure outlined within this SOW accordingly; provided, however, that such fee structure changes, if any, must be reasonable, proportional to the changes in such technical specifications. |
| 11. | Limitations of Data Accuracy. Both parties acknowledge that the accuracy and completeness of the Services may be limited by inaccuracies and incompleteness, if any, within data provided by Client to Inovalon. |
Master Services Agreement
Statement of Work #3 – CAAS Services
Page 7 of 7
Schedule 1 to Statement of Work #3
CMS RISK ADJUSTMENT DATA SUBMISSION
DATA SHEET
CMS Data Submitter Information
|
Plan Number (Hnnnn):
|
|
|
Plan Name:
|
|
|
Address:
|
|
|
Fax Number:
|
|
|
Operations Contact Person:
|
|
|
E-mail address:
|
|
|
Phone Number:
|
|
|
Technical Contact Person:
|
|
|
E-mail address:
|
|
|
Phone Number:
|
Inovalon Process Information
|
Date of First Inovalon CMS Submission:
|
|
Initials:
|
|
|
Date:
|
|
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 1 of 14
Statement of Work #4
CLAIMS & PAYMENT INTEGRITY
RETROSPECTIVE MEDICARE ADVANTAGE RISK ADJUSTMENT
(Known as Capitation Risk Adjustment, or CARA®, services)
This Statement of Work #4 (this “SOW”) is entered into and effective as of January 1, 2016 (the “SOW Effective Date”) pursuant to the terms and conditions of that certain Master Services Agreement dated January 1, 2016 (as amended, the “Agreement”) by and between Inovalon, Inc. (“Inovalon”) and Triple-S Advantage, Inc., (“TSA”), administered by Triple- S Advantage Solutions, Inc. (“Client”). Inovalon will use all commercially reasonable efforts to provide the following CARA® services (the “Services”) to Client in a professional and workmanlike manner.
| 1. | Definitions. For the purposes of this Agreement, in addition to the common process definitions set forth in Section 3(d) below applicable to the specific CARA Processes outlined in Section 3 (Service Segments), the following terms are defined as follows: |
| a. | “Member Population” shall mean the group of members comprised of the enrollees within the Medicare Advantage product line of Client for which Services are to be rendered, as designated by Client. Inovalon and Client agree that Inovalon will be the sole third party vendor only for the provision of the contracted Services for the Member Population as outlined in this SOW. With respect to the Member Population, Client may, at its discretion, complement or pursue additional initiatives using other contractors, but, Client agrees to share with Inovalon the results of any such complementary services. For clarity, such complementary services will not be in lieu of or decrease from the Services provided by Inovalon. Additionally, nothing in this definition prevents Client from revoking delegated Services in the event of a breach on the part of Inovalon. Client shall supply Inovalon with identifying information for those individual members included in the Member Population. Client has the right to exclude Medicare Advantage members from the Member Population, subject to the limitations described below. Client will ensure that the Member Population meets the minimum requirements listed below. Client will define the Member Population by providing Inovalon with written notice of a preliminary percentage estimate by October 1st preceding the applicable calendar year, a final percentage by November 1st preceding the applicable calendar year, and the actual members within the Member Population within one week of December 7th preceding the applicable calendar year. The parties acknowledge that the flexibility to define the Member Population may affect the ability of Inovalon to meet certain return on investment provisions in a particular SOW, and this will be taken into consideration when measuring the return on investment requirements. |
| i. | For the calendar year 2016, the Member Population shall be comprised of no less than sixty-five percent (65%) of Client’s total then-current Medicare Advantage membership. |
| ii. | For the calendar year 2017, the Member Population shall be comprised of no less than fifty-five percent (55%) of Client’s total then-current Medicare Advantage membership |
| b. | “CEDI Identification Logic” shall mean that set of proprietary, clinically-driven algorithms within the solution used to identify data which suggests evidence of a gap between existing documentation and that documentation needed to accurately reflect a member’s HCC-driven reimbursement factor. These incongruences between documented encounter data (used by CMS for reimbursement calculations) and data suggesting the existence or required validation of chronic, additional, worsening, or more accurately classified disease processes that are not already within the standard claims coding system of Client (as would be submitted to CMS) are referred to as “Clinical Encounter Data Incongruences” or “CEDIs”. The CEDI Identification Logic is a proprietary process and is a component, along with all proprietary data sets utilized thereby, of Inovalon Intellectual Property. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 2 of 14
| c. | “Target CEDI” shall mean a clinical encounter data incongruence (CEDI) which is identified during the processing of Health Plan Data Sets (defined below), with the application of the Inovalon CEDI Identification Logic suggesting the existence of chronic, additional, worsening, or more accurately classified disease processes that is not already documented within the standard claims coding system of Client (as would be submitted to CMS). |
| d. | “Field CEDI” shall mean a clinical encounter data incongruence (CEDI), other than a Target CEDI, which is identified during review of a member’s medical record data that is found to be a chronic, additional, worsening, or more accurately classified disease processes that is not already documented within the standard claims coding system of Client (as would be submitted to CMS). |
| e. | “CEDI Member” shall mean an enrollee (or member) of a Client health plan identified through the application of Inovalon’s CEDI Identification Logic as having one or more claims and encounter data incongruence(s) which are believed to substantiate the existence of an uncoded, under-coded, mis-coded, or ineligibly coded impact on past, current, or future reimbursement rates. |
| f. | “CEDI Member Medical Record” shall mean any unique and individual medical record pertaining to a CEDI Member. |
| g. | “ChaseWise” shall mean that process proprietary to Inovalon that enables an efficient ordering of CEDI Member Medical Records, available practitioners, and associated site locations designed to facilitate a highly cost-effective prioritization of potentially contributing practitioners, medical records, and medical record locations. |
| h. | “Factor Change Potential” or “FCP” shall mean that amount of difference between a member’s known factor and associated HCC and that determined to be potentially represented within identified CEDI(s). |
| i. | “FCP Threshold” shall mean that amount of Factor Change Potential determined by Client to be necessary to justify the pursuit of a medical record review of a CEDI Member Medical Record. For purposes hereof, a maximum FCP Threshold will be set at 0.10 (the “Maximum Reasonable FCP Threshold”). While Client may in its discretion set the FCP Threshold to any value (greater or less than 0.10) for purposes of managing the pursuit and verification of medical records by medical record review processes, as detailed in this SOW, for the purposes of the CEDI Identification Fee calculation provided in Section 6 below, such FCP Threshold will be interpreted as being no higher than the Maximum Reasonable FCP Threshold. |
| j. | “Probability Threshold” shall mean that level of sensitivity determined by Client to be necessary to justify the pursuit of a medical record review of a CEDI Member Medical Record. The Probability Threshold can be set at high, medium, low, or very low. Unless set by Client at a different level the default Probability Threshold will be “medium”. While Client may in its discretion set the Probability Threshold to any value (high, medium, low, or very low) for purposes of managing the pursuit and verification of medical records by medical record review processes as detailed in this SOW, for the purposes of the CEDI Identification Fee calculation provided in Section 6 below, such Probability Threshold will be interpreted as being no higher than “medium” setting. As used herein, the Probability Threshold and the FCP Threshold will be collectively referred to as the “CARA Thresholds”. |
| k. | “Health Plan Data Set” shall mean files for the Member Population as more specifically identified in Section 4(a)(iv) and as may be provided by Client in raw native format, including such items as member demographics, member product enrollment segments, provider demographics, provider service claims, provider encounters and diagnoses, member laboratory results, pharmaceutical prescription claims, and public data repository and registry files. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 3 of 14
| l. | “CARA Medical Record Chase Data Set” shall mean that data set which consists of member, medical record location, and provider information associated with the medical records of identified Eligible Target CEDI Members (see Section 3(b)(vii)(2)), as well as specific claims and encounter data incongruence details, so as to enable the review of such medical records by a medical record reviewer in an effort to substantiate suspected disease and/or co-morbidity states for accurate HCC factor score rates. |
| m. | “MRR Data Set” shall mean that data set which contains the abstraction results of any medical record reviews conducted by Inovalon. |
| n. | “Member Disease State Profile” shall mean the set of all known disease conditions eligible for CMS or State Department of Health reimbursement under the HCC CRG, CDPS, ACG, or DxCG, as the case may be, coding system for a specific member, as well as relevant supporting data and associated encounter and/or claim dates. |
| o. | “Fully Integrated EMR” means an electronic medical record (EMR) with which Inovalon’s technology platform is fully integrated such that medical record data can be identified and abstracted directly from the EMR in a predetermined format without the need to manually identify, extract, and process each document. For the sake of clarity, this does not include the remote or onsite extraction of an EMR record from the front end of the EMR platform (such as screen scraping from an EMR or printing or exporting EMR records to paper or some format). |
| p. | “Traditional Medical Record Data Collection” means the use of traditional medical record data collection methodologies (e.g., paper-based medical record data collection, or any other non-Fully Integrated EMR methodology). Traditional Medical Record Data Collection includes printing or exporting EMR records to paper or some format. |
| 2. | Term and Termination. This SOW shall commence on the SOW Effective Date and shall continue in effect through December 31, 2017 (the “Term”) and then continue in accordance with the Transition Services described in Section 3. |
| a. | Termination Option in the Event of Demonstration of Limited Benefit. Provided Client has reasonably satisfied its obligations hereunder, Client will have a right to terminate this SOW (a) January 31, 2017 (the “Initial Termination Option Date”) following the conclusion of the first full cycle of Processes performed hereunder, and (b) the date of each anniversary of the Initial Termination Option Date (each, an “Annual Termination Option Date”) (the Initial Termination Option Date and each Annual Termination Option Date referred to as a “Termination Option Date”), in the event that the aggregate reimbursement improvement resulting from Processes does not exceed three times the cost of the total fees paid to Inovalon in respect to such Processes, calculated as the total financial impact as evidenced in Inovalon’s CARA Results Reporting and Data (described below). Each successive termination right will expire upon the earlier of (i) 15 days after the respective Termination Option Date, or (ii) the date Client notifies Inovalon of its desire to continue with the Services contemplated herein. For the avoidance of doubt, in the event that Client does experience aggregate reimbursement improvement resulting from the Processes hereunder in excess of three times the cost of the total fees paid to Inovalon in respect to such Services, or as each limited termination right provided under this Section 2 expires, the term of this SOW will remain in effect and such termination right will become null and void. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 4 of 14
| 3. | Transition Services. In the event of termination or expiration of the Agreement and with respect to Client’s Medicare Advantage Members who will no longer be part of the Member Population effective January 1 of a contract year in accordance with the process outlined in Section 1(a), Inovalon will provide the support described below up until the end of the Transition Period (defined as 3 the month period following (a) the Termination Date or (b) January 1 with respect to Client’s Medicare Advantage members who are not part of the Member Population in accordance with the process outlined in Section 1(a),) both (A) in accordance with all standards set forth in the Agreement and this SOW and (B) with the same level of accuracy, intensity and timeliness of Services performed before receipt of the notice of termination or non-renewal, meeting all the data specifications required by Client and CMS. |
| i. | The Term (as defined in Section 2) will continue through March 31, 2018 (the “Termination Date” for purposes of this SOW), the FRO Process CMS Submission Deadline. Inovalon will not begin any new CARA Processes in 2018 but will complete those CARA Processes launched in 2017. |
| ii. | Inovalon will perform clinical coding and HCCs abstraction for all medical records received through the process then underway upon the Termination Date within 90 days following the process underway on the Termination Date; |
| iii. | Inovalon will make available RAPs files and EDS files for medical records coded and abstracted during the final process by the earlier of (1) the CMS submission deadline or (2) 90 days following the end of the process; and |
| iv. | Inovalon will make available to Client (by uploading to a secure depository designated by Client or through other methods mutually agreed upon by the parties) all Medical Records received within 90 days following the process underway on the Termination Date. |
| 4. | Service Segments. Inovalon will provide services to Client consisting of those components identified in this Section 3 of this SOW. |
| a. | Future Reimbursement Accuracy Optimization Processes (“FRO Processes”): Inovalon will utilize Health Plan Data Sets to perform CARA processes on a 12-month date of service period (a “FRO Process DOS Period”) utilized for the submission of data to CMS (on or before the respective deadline, referred to as the respective “FRO Process CMS Submission Deadline”) for the setting of reimbursement rates for a respective Future Reimbursement Payment Period (each a “FRO Process Payment Period”). |
| i. | Each FRO Process DOS Period consists of a period of 12 consecutive calendar months, beginning either on January 1st or July 1st of each year. The FRO Process associated with the FRO Process DOS Periods beginning on January 1st will be referred to as the “FRO 1 Process” and the FRO Process associated with the FRO Process DOS Periods beginning July 1st will be referred to as the “FRO 2 Process.” The first FRO Process DOS Period for which CARA processes are to be undertaken under this Agreement is: 1/1/15 to 12/31/15. |
| ii. | Each FRO Process CMS Submission Deadline occurs on the first Friday in March (for FRO Process DOS Periods ending the preceding December 31st) or the first Friday in September (for FRO Process DOS Periods ending the preceding June 30th), as the case may be, following the respective FRO Process DOS Period. For sake of example, the FRO Process CMS Submission Deadline for the submission of all data associated with the first FRO Process DOS Period processed under this Agreement is: 3/4/16. |
| iii. | Each review of a FRO Process DOS Period and data submitted by the respective FRO Process CMS Submission Deadline is utilized by CMS to set reimbursement rates for the Client for the next full six consecutive month period (i.e., either January through June or July through December, as the case may be). For sake of example, the period for which the first FRO Process DOS Period processed under this Agreement impacts reimbursement (the respective FRO Process Payment Period) is: 7/1/16 to 12/31/16. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 5 of 14
| iv. | The CARA FRO Processes period associated with each FRO Process DOS Period (each a “CARA FRO Processes Period”) begins on the 15th day of the twelfth month of the respective FRO Process DOS Period and concludes on the respective FRO Process CMS Submission Deadline. For sake of example, the first CARA FRO Processes Period will generally begin 12/15/15 (or upon commencement of this Agreement, as the case may be) and would conclude on the first FRO Process CMS Submission Deadline, namely 3/4/16. |
| v. | The combination of each respective FRO Process DOS Period, FRO Process CMS Submission Deadline, FRO Process Payment Period, and associated CARA FRO Processes Period is referred to as the respective “FRO Process Cycle”. Figure 1 below presents a graphical rendition of four FRO Process Cycles. |
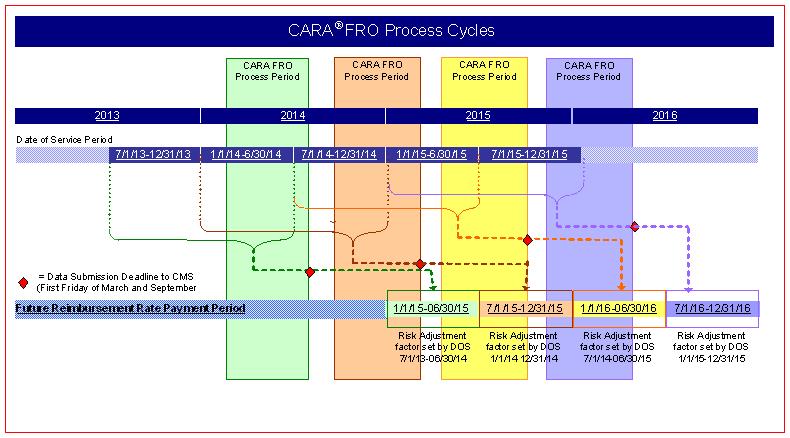
Figure 1: Future Reimbursement Accuracy Optimization (FRO) Process Cycles
| b. | Reconciliation Reimbursement Accuracy Optimization Processes (“RRO Processes”): Inovalon will utilize Health Plan Data Sets to perform CARA processes on a 12-month date of service period (each a “RRO Process DOS Period”) utilized for the submission of data to CMS (on or before the respective deadline, referred to as the respective “RRO Process CMS Submission Deadline”) for the setting of final reconciliation reimbursement for the respective RRO Payment Period (each a “RRO Process Reconciliation Period”). |
| i. | Each RRO Process DOS Period consists of a full calendar year beginning on January 1st and ending December 31st of the same year. The first RRO Process DOS Period for which CARA processes are to be undertaken under this Agreement is: 1/1/15 to 12/31/15. |
| ii. | Each RRO Process CMS Submission Deadline occurs on second January 31st following the respective RRO Process DOS Period (i.e. the end of the 13th month following the end of the RRO Process DOS Period). For sake of example, the RRO Process CMS Submission Deadline for the submission of all data associated with the first RRO Process DOS Period is: 1/31/17. |
| iii. | Each review of a RRO Process DOS Period and data submitted by the respective RRO Process CMS Submission Deadline is utilized by CMS to set final lump-sum reimbursement for Client for the RRO Process Reconciliation Period. For sake of example, the period for which the first RRO Process DOS Period impacts final reimbursement (the respective RRO Process Reconciliation Period) is: 1/1/16 to 12/31/16. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 6 of 14
| iv. | The CARA RRO Processes period associated with each RRO Process DOS Period (each a “CARA RRO Processes Period”) is sought to be distributed over as broad a period as possible for maximal efficiency and outcome benefit and, as such, begins during the second half of April of the respective RRO Process Reconciliation Period and concludes on the respective RRO Process CMS Submission Deadline. For sake of example, the first CARA RRO Processes Period will generally begin 4/15/16 (or upon the SOW Effective Date, as the case may be) and will conclude on the first RRO Process CMS Submission Deadline, namely 1/31/17. |
| v. | The combination of each respective RRO Process DOS Period, RRO Process CMS Submission Deadline, RRO Process Reconciliation Period, and associated CARA RRO Processes Period is referred to as the respective “RRO Process Cycle”. Figure 2 below presents a graphical rendition of two RRO Process Cycles. |
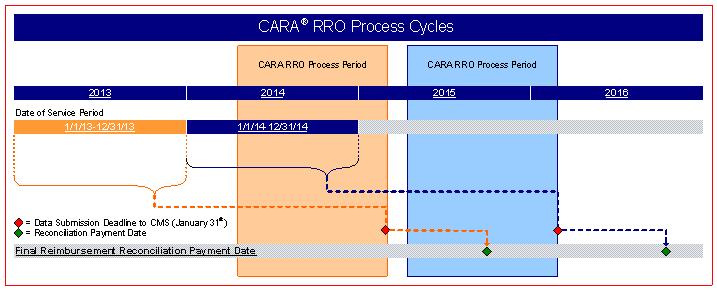
Figure 2: Final Reconciliation Reimbursement Accuracy Optimization (RRO) Process Cycles
| c. | Common Process Definitions: The following are definitions common to each of the processes outlined within Sections 3(a) and 3(b) of this SOW. |
| i. | The combination of the FRO Processes and RRO Processes will together be referred to as the “CARA Processes”, and will individually be referred to each a “CARA Process”; |
| ii. | The CARA Process date of service periods, FRO Process DOS Period and RRO Process DOS Period will together be referred to as the “CARA Processes DOS Periods”, and will individually be referred to each the respective CARA Process’ “CARA Process DOS Period”; |
| iii. | The CMS deadlines, FRO Process CMS Submission Deadlines and RRO Process CMS Submission Deadlines, will together be referred to as the “CARA Processes CMS Submission Deadlines”, and will individually be referred to each the respective CARA Process’ “CARA Process CMS Submission Deadline”; and |
| iv. | The CARA Process Periods, the CARA FRO Process Periods and the CARA RRO Process Period will collectively be referred to as the “CARA Processes Periods”, and will individually be referred to each the respective CARA Process’ “CARA Process Period”. |
| 5. | Inovalon CARA Data Processing Responsibilities. Inovalon will provide services to Client consisting of the following components: |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 7 of 14
| a. | Project Initiation Activities & General Project Management. Inovalon will undertake the following steps in preparation for the CARA administrative data processing: |
| i. | Project Integration Call: Inovalon will schedule and coordinate a project integration call with Client during which the following materials and topics will be provided, introduced, and addressed: |
| 1. | Inovalon Contact Information: Team contact information for primary Inovalon project personnel and support escalation protocols will be provided to Client; |
| 2. | CARA Project Plan: A comprehensive CARA project plan will be provided to Client which will include data delivery schedules, Inovalon deliverables, and Client deliverables; and |
| 3. | CARA Project Questionnaire: A questionnaire identifying key information requirements by Inovalon of Client (such as the clarification of Client IT personnel contact information, database characteristics, and other such applicable details) will be provided by Inovalon to Client with concrete follow-up completion and timeline requirements. |
| ii. | CARA System Training: Inovalon will schedule, coordinate, and conduct CARA Reporting & Analytics system training for designated Client personnel consisting of instructions for accessing: |
| 1. | Client Web Portal functions; |
| 2. | Financial Impact Reporting; |
| 3. | Management of CARA Thresholds; and |
| 4. | Process Reporting & Analytics. |
| iii. | Establish Joint Schedule: Based on the information gained from the Project Integration Call (Section 4(a)(i) above) and information returned to Inovalon within the CARA Project Questionnaire, Inovalon will establish and conduct a mutually agreed upon comprehensive schedule for conference calls (generally bi-weekly ) for, amongst other issues, the: |
| 1. | Provision of project status reports; |
| 2. | Review and reconciliation of CARA Project Plan activities; |
| 3. | Review of issue tracking reports (if any) and respective resolution of status; and |
| 4. | Identification and discussion of new issues for resolution (if any). |
| iv. | Specification of Data Requirements: Based on the information gained from the Project Integration Call (Section 4(a)(i) above) and information returned to Inovalon within the CARA Project Questionnaire, Inovalon will provide Client with a comprehensive outline of data required by Inovalon for the CARA administrative data processing of the Member Population (which will constitute the Health Plan Data Set for the Member Population and which shall be updated from time to time) including, amongst other data, the: |
| 1. | Member demographics data; |
| 2. | Member historical HCC data; |
| 3. | Member historical factor data; |
| 4. | Member claims and cost data; |
| 5. | Member enrollment data; |
| 6. | Member laboratory data; |
| 7. | Member pharmacy and cost data; |
| 8. | Member procedure data; |
| 9. | Member durable medical equipment data; |
| 10. | Payment agent-specific data such as: |
| a. | Medicare Advantage data such as: |
| i. | RAPS & RAPS return data; |
| ii. | MOR detail data; |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 8 of 14
| iii. | MMR detail data; |
| iv. | CMS bid data; |
| v. | EDS submission & response files; |
| b. | Managed Medicaid data such as: |
| i. | Electronic submission file data (e.g. MEDS II, MEDS III, eData, etc.); |
| ii. | State bid, factor, and rate data; |
| c. | Commercial data such as: |
| i. | Monthly premium data. |
| 11. | Care provider data. |
| b. | Performing CARA Data Processing & Management. For each of the CARA Processes and for each Member Population, Inovalon will undertake the following CARA processing services based upon clinical best practices, designated cost-benefit thresholds, and in accordance with CMS HCC technical specifications (as may be revised by CMS from time to time): |
| i. | Providing assistance to designated Client personnel in the provision of Health Plan Data Sets to Inovalon via secure FTP portal (or alternate method as mutually agreed to between Inovalon and Client); |
| ii. | Coordinating and leading native data mapping conference calls with designated Client personnel to resolve data inconsistencies revealed during Inovalon data validation processes; |
| iii. | Implementing data mapping processes to facilitate import of Health Plan Data Sets; |
| iv. | Establishing historical and current rate factors for each Member based upon member demographics and relative HCCs known to Client as provided within Health Plan Data Sets; |
| v. | Establishing historical and current member capitation rates based upon member demographics and HCCs known to Client as provided within Health Plan Data Set; |
| vi. | Applying Inovalon’s CARA processes to Health Plan Data Sets pertaining to the respective Process DOS Period to identify candidate Target CEDIs; |
| vii. | Cross-referencing identified candidate Target CEDIs against each respective member’s known Member Disease State Profile to identify previously unsubstantiated disease states (the “Newly Identified CEDI Disease States”); |
| viii. | Filtering candidate Target CEDIs that have been found to represent Newly Identified CEDI Disease States against established Client CARA Thresholds to identify members eligible for follow-up medical record review investigation (the “Eligible Target CEDI Members” and their respective CEDIs, “Eligible Target CEDIs”); |
| ix. | Formulating CARA Medical Record Chase Data Sets consisting of relevant Eligible Target CEDI Members; |
| x. | Prioritize CARA Member Medical Records within CARA Medical Records Chase Data Sets via the application of Inovalon’s ChaseWise medical record chase order classification logic; |
| xi. | Coordinate CARA Medical Record Review (MRR) Data Exchanges & Integration as outlined within Section 4(c) below; |
| xii. | Providing comprehensive reporting of CEDI Members, associated medical record review findings, financial impact results, and information on coding improvement opportunities to Client; |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 9 of 14
| xiii. | Generate and provide to Client a Risk Adjustment Processing System (RAPS) file and EDS file (the “RAPS File”) for review by Client and submission, in whole or in part at the sole discretion of Client, to CMS on or before the respective FRO Process CMS Submission Deadline or RRO Process CMS Submission Deadline, as the case may be; and |
| xiv. | Establishing updated Member Disease State Profiles based upon integrated results of resulting MRR Data Set. |
| c. | Coordinate CARA Medical Record Review (MRR) Data Exchanges & Integration. Inovalon will provide services with respect to any necessary medical record reviews, which will be fully coordinated and managed by Inovalon. Inovalon will manage all necessary medical record reviews as follows: |
| i. | Inovalon will facilitate the cleaning of the CARA Medical Record Chase Data Set in seeking to clarify the physical location of sought CEDI Member Medical Records (the “CEDI Member Medical Record Site”); |
| ii. | Inovalon will contact valid CEDI Member Medical Record Sites, provide evidence of authorization for sought medical record reviews, and coordinate efficient scheduling of identified CEDI Member Medical Records; |
| iii. | Inovalon will undertake the request, remote and/or onsite review of identified CEDI Member Medical Records seeking to substantiate and/or further clarify the existence or absence of disease processes suspected within the respective identified Target CEDI, and subject to the availability of such CEDI Member Medical Record, a separate medical record review will be performed for each applicable Target CEDI within each such medical record (i.e., each unique Member/Target CEDI/Provider medical record combination which is reviewed is done so as a separate and unique medical record review); |
| iv. | Inovalon will digitize relevant medical record components that substantiate the findings as outlined in 4(c)(iii) above unless digitizing is not permitted at the time of the onsite review by the CEDI Member Medical Record Site; |
| v. | Inovalon will provide to Client all reviewed medical record results and substantiating digital scans of relevant medical record components; |
| vi. | Inovalon will collect and will provide to Client a copy of all medical records collected as part of the HCCs abstraction for risk adjustment purposes; |
| vii. | Inovalon will give the option to providers to deliver medical records by mail, fax, or secure FTP or secure thumb drive; |
| viii. | Each month Inovalon will review all suspected Members that require a medical record to be reviewed; and |
| ix. | Inovalon will provide to Client a monthly report containing providers by Alianza (defined as an administrative entity organized under the laws of the Commonwealth of Puerto Rico, engaged in the business of providing primary healthcare services disclosed to Inovalon through the Health Plan Data Set), number of medical records requested and number of medical records received. |
| d. | Provision of CARA Results Reporting and Data. |
| i. | Process Reporting: Providing Member Population process-level progress reporting, financial/HCC impact summary result reporting, chronological financial/HCC impact results comparison reporting; |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 10 of 14
| ii. | CARA Member Reporting: Providing Member Population member-level reports by HCC for review and validation of results by Client; |
| iii. | Member-Level Reporting: Providing member-level reporting for each HCC, each medical record review report, and medical record component details to facilitate Client’s claims audit, claims adjustment, and risk adjustment processes; and |
| iv. | Summary Reporting: Providing CEDI process reporting for executive level summary statistics regarding project management, process findings, and financial impacts. |
| e. | Service Level Agreements (SLAs). |
| i. | Timeline for processing Medical Records For all medical records collected, Inovalon agrees to review, code and process each such that 90% of the volume (the “Minimum Commitment”) is ready for the subsequent RAPS file and EDS file within twenty (20) business days. Exceptions to this are when a volume of records greater than 10,000 is received in a given week. |
| 1. | Method of Determination of SLA Performance. This SLA will be measured on a monthly basis. |
| 2. | Consequences of Failure to Meet SLA. Inovalon will be penalized five percent (5%) of the MRR Fee for each medical record that fails to meet the Minimum Commitment. |
| f. | Optional CARA RRO Recharge Process. In addition to the Services described in this SOW in an effort to apply incremental resources on improving the risk score accuracy pertaining to a particular date of service period), Client may request that Inovalon undertake a rerunning of analytics for the purpose of identifying additional CEDIs and corresponding medical records for review (each rerunning, a “RRO Process Recharge”). Upon mutual consent, Inovalon will perform the RRO Process Recharge and will invoice the fees for such additional CEDIs as described in Section 6(a)(ii) of this SOW and Inovalon will invoice any corresponding medical record reviews as described in Section 6(a)(iii) of this SOW. There is no additional CARA Base Processing Fees charged in association with any such RRO Process Recharge. |
| 6. | Client CARA Administrative Data Processing Responsibilities: Client will provide process support to Inovalon consisting of: |
| a. | Project Initiation Activities & General Project Management. |
| i. | Designating Client internal personnel for, and participation in, Project Integration Call as outlined in Section 4(a)(i) above; |
| ii. | Providing project initiation materials to Inovalon as requested by Inovalon, including, amongst other items: |
| 1. | Identification of those personnel at Client who are to be involved with the CARA administrative data processing project, including contact information, clarification of rolls, and related roll support escalation protocols; |
| 2. | Completion of the CARA Project Questionnaire as provided by Inovalon to Client within seven calendar days (or longer period of time as may be mutually agreed to by Inovalon and Client) of provision by Inovalon; and |
| 3. | Feedback on CARA Project Plan including production schedules, Inovalon deliverables, Client deliverables, and production milestone expectations, and written acknowledgement of plan within seven calendar days (or longer period of time as may be mutually agreed to by Inovalon and Client) of provision by Inovalon. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 11 of 14
| iii. | Designating Client internal personnel for, and participation in, CARA System Training as outlined in Section 4(a)(ii) above; |
| iv. | Designating Client internal personnel for, and participation in, conference calls between Inovalon and Client, occurring at least bi-weekly (i.e. every other week), regarding the status and schedule of CARA Administrative Data Processing services as outlined in Section 4(a)(iii) above; and |
| v. | Monitor and review decision factors underlying the CARA Processes, including particular prioritization rules relevant to the ChaseWise ordering protocols and CARA Threshold determinations, and provide Inovalon with confirmations and appropriate authorizations of default options or alternative selections, as the case may be. |
| b. | Performing CARA Administrative Data Processing & Management. For each of the CARA Processes and for each Member Population, Client will undertake the following responsibilities: |
| i. | Providing necessary complete Health Plan Data Sets to Inovalon via secure FTP portal (or alternate method as mutually agreed to between Inovalon and Client) on or before the 10th day of each month (the “Health Plan Data Set Due Date”); |
| ii. | Providing complete and accurate (to the best of Client’s knowledge) documentation to Inovalon pertaining to definitions of all file fields and mapping of all proprietary codes utilized in the Health Plan Data Set; |
| iii. | Designating Client internal personnel for, and participation in, native data mapping conference calls with Inovalon as outlined in Section 4(b)(iii) above; |
| iv. | Providing assistance in the resolution of native data mapping inconsistencies revealed during Inovalon data validation processes as outlined in Section 4(b)(iii) above; and |
| v. | Providing to Inovalon all necessary baseline member demographics, known HCCs, and established factors for calculating baseline capitation rates as outlined in Section 4(b)(iv) above. |
| c. | Coordinate CARA Medical Record Review (MRR) Data Exchanges & Integration. Client will be responsible for the following items related to the medical record review process: Identification and determination of CARA Thresholds for utilization in creation of CARA Medical Record Chase Data Sets for each Member Population (as such CARA Thresholds will be determined by Client via execution of a CARA Factor & Probability Threshold Selection Form in association with each CARA Process; provided, however, that in the event that such Form is not delivered by Client to Inovalon within 10 days of Inovalon’s request therefor, Inovalon will proceed with the default FCP Threshold of 0.10 and Probability Threshold of “medium” for such CARA Process). Additionally, Client is responsible for working through and resolving the issues with CEDI Member Medical Record Sites on the issues log available via the Client Web Portal (the “Issues Log”) to ensure cooperation by CEDI Member Medical Record Sites. |
| d. | Supporting CARA Results Reporting and Data Submissions. Coordinating with Inovalon to investigate and resolve potential errors or data inconsistencies. |
REIMBURSEMENT AND PAYMENT SCHEDULE
FOR DATA PROCESSING SERVICES
| 7. | CARA Administrative Data Processing Fees. |
| a. | Process Fees: For the services outlined within this SOW, Inovalon will charge and invoice Client as follows: |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 12 of 14
| i. | CARA Processes Fees: Inovalon will charge a base fee for each CARA Process performed on each Member Population (the “CARA Processing Fees”) as outlined in Table 1 below. The CARA Processing Fee will be invoiced at the initiation of the respective CARA Process Period and will be based on the Member Population from the Health Plan Data Set processed for the applicable CARA Process. |
|
Member Population
|
Population
Members
Enrolled
|
CARA
Processing
Fee
|
|
Triple-S Advantage, Inc. (H4005)
|
121,743
|
$ 39,823.53
|
|
$ 19,950
|
Table 1: CARA Processing Fees
| ii. | CEDI Identification: Inovalon will charge a fee (the “CEDI Identification Fee”) equal to $20.46 for each Eligible Target CEDI and each Field CEDI identified through the provision of the CARA Processes. The sum of any CEDI Identification Fees will be invoiced to Client monthly in arrears. |
| iii. | Medical Record Review Fees: Inovalon will charge a fee for each Target CEDI medical record review performed by Inovalon (the “MRR Fees”) equal to i) a fee (the “Medical Record Review Fee”) equal to 27.09 per each medical record review performed, plus ii) a mileage reimbursement (the “Mileage Reimbursement”) equal to the sum of all mileage incurred in the medical record review process multiplied by the IRS mileage reimbursement rate. The sum of any MRR Fees will be invoiced to Client monthly in arrears. Additionally, in the event that a Medical Record Review is conducted through a Fully Integrated EMR and not a Traditional Medical Record Data Collection methodology (e.g., paper-based medical record data collection, or printing or exporting EMR records to paper or some format) the MRR Fee for each such review conducted through a Fully Integrated EMR will be equal to $21.77. |
| b. | Pass-Through Fees: Inovalon will charge to Client the cost for the pass-through items at cost, each of which shall be outlined in reasonable detail by Inovalon (the “Pass-Through Fees”). Examples of pass-through items are UPS and FedEx fees. |
| 8. | Provision of Support Services. Client may, in its sole discretion, utilize Support Units in any proportion for the provision by Inovalon of support services, as the case may be. Inovalon will invoice Client for the Support Units in arrears at the price of $50 per Support Unit. Client may elect to use the Support Units for Client IT / CARA integration support and/or client operations process improvement consulting services and Inovalon agrees to provide to Client IT / CARA integration support and/or client operations process improvement consulting services (“Support Services”). In the event that a Client request for Support Services is expected to incur Support Units, Inovalon will provide a good faith estimate to Client and receive Client’s written approval prior to beginning such work related to such request for Support Services |
| a. | Support Units are determined based on the following levels of support. |
| i. | Level 1 Support: Support questions regarding basic technical questions which are not product specific (e.g. questions regarding logging into the Inovalon Client Web Portal). An example of Level 1 Support (which is always included) is technical assistance in accessing ePASS or the Client Web Portal. |
| ii. | Level 2 Support: Support questions which are product-specific such as day-to-day functionality, reporting, and use, specific to the CARA solution, services, and/or subject matter and which are considered basic in their complexity as well as product-specific training. An example of Level 2 Support (which is always included) is the daily operational support of the client services organization including reviewing the Prospective Advantage Financial Impact Report, or product specific training such as CARA issues log training. |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 13 of 14
| iii. | Level 3 Support: Support questions which are product-specific (i.e. specific to the CARA solution, services, and/or subject matter) and which are considered advanced in their complexity, but which do not require a senior management person’s involvement (i.e. not requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 3 Support is generating a specific financial report investigating particular HCC’s or medical conditions by a particular medical group. |
| iv. | Level 4 Support: Support questions which are product-specific (i.e. specific to the CARA solution, services, and/or subject matter) and which are consider highly advanced in their complexity, therefore requiring (or, at the request of the Client, involving) a senior management person’s involvement (i.e. not requiring a: product leader, Senior Director (or higher), or Medical Director). An example of Level 4 Support is performing a risk adjustment accuracy project which compares found HCC’s by a specific medical group on a year over year basis. |
| b. | Support Units are calculated based on the amount of time and the level of support utilized as set forth in Table 2 below. |
|
Support Level
|
Number of Units /
Hour
|
Cost by the Hour*
|
|
Level 1
|
Included within the scope of Services
|
|
|
Level 2
|
Included within the scope of Services
|
|
|
Xxxxx 0
|
0
|
x 000
|
|
Xxxxx 4
|
6
|
$ 300
|
Table 2: Support Units
* Level 3 and Level 4 are calculated in hourly increments.
| 9. | General Invoicing. Except as otherwise provided above, Inovalon will invoice Client for the Services provided on a monthly basis in arrears. Inovalon will provide to Client a detailed invoice outlining all costs related to medical record reviews broken down by category and measurement unit. Subject to Inovalon’s compliance with the provisions of this SOW and the Agreement, Client will pay Inovalon for medical record reviews and associated expenses and other out-of-pocket reasonable expenses incurred by Inovalon as part of these services, provided that all such expenses with the exception of mileage and print fulfillment expenses must be pre-approved by Client in advance of being incurred and that all such expenses do not exceed more than TEN PERCENT (10%) of the total aggregate services fees for these services. Inovalon shall provide appropriate vouching documentation for all expenses. |
| 10. | Initial CARA Processes & Delay Impact on Medical Record Review Processes. It is acknowledged that the initial cycle of CARA Processes covered under this Agreement are impacted by any constraint of process time, including the date the Agreement is executed and delivered and the date proper Health Plan Data Sets are delivered to Inovalon. Moreover, Client understands and acknowledges that Inovalon will dedicate specific resources and enter into particular commitments in reliance upon the respective obligations and commitments made by Client hereunder, and that each delay caused by Client has a material impact on Inovalon. As such: |
| a. | In the case that either i) the execution date of this Agreement is later than the start of one or more CARA Process Periods, or ii) necessary and complete Health Plan Data Sets are not provided to Inovalon by the respective CARA Process’ Health Plan Data Set Due Date, Inovalon will make reasonable efforts to try to minimize the impact of Client’s delay on service delivery, however Inovalon’s support or provision obligations (as the case may be) of necessary medical record reviews as outlined under Section 4(c) of this SOW will necessarily be on a “best efforts” basis for such respective CARA Processes; and |
Master Services Agreement
Statement of Work #4 –Capitation Risk Adjustment (CARA®) Scope of Services
Page 14 of 14
| b. | In the case that Client, in its discretion and at no fault of Inovalon, requires Inovalon to delay or temporary halt support or provision of necessary medical record reviews as outlined under Section 4(c) of this SOW either i) during such medical record review processes, or ii) preceding such medical record reviews processes such that the initiation of medical record reviews is delayed, Client will pay to Inovalon a fee (the “Client Interruption of Service Fee”) equal to 50% of the amount of MRR Fees that would have been due for such medical record reviews which Inovalon staffed and that would have been performed during such delay or temporary halt (calculated by the number of targeted medical record reviews divided by the originally planned medical record review period’s number of business days). |
| 11. | Specification Changes. In the event that CMS should materially change the risk adjustment reimbursement technical specifications, Inovalon reserves the right to adjust the fee structure outlined within this SOW accordingly; provided, however, that such fee structure changes, if any, must be reasonable, proportional to the changes in such technical specifications. |
| 12. | Limitations of Data Accuracy. Both parties acknowledge that the accuracy and completeness of the Services may be limited by inaccuracies and incompleteness, if any, within data provided by Client to Inovalon. |


