CONTRACT NUMBER: FA- 07-16936-00
AMENDMENT NUMBER 8
MIDDLE GRAND REGION
CONTRACTOR RISK AGREEMENT
BETWEEN
THE STATE OF TENNESSEE,
d.b.a. TENNCARE
AND
AMERIGROUP TENNESSEE, INC.
CONTRACT NUMBER: FA- 00-00000-00
For and in consideration of the mutual promises herein contained and other good and valuable consideration, the receipt and sufficiency of which is hereby acknowledged, the parties agree to clarify and/or amend the Contractor Risk Agreement (CRA) by and between the State of Tennessee TennCare Bureau, hereinafter referred to as TENNCARE, and AMERIGROUP TENNESSEE, INC., hereinafter referred to as the CONTRACTOR as specified below.
Titles and numbering of paragraphs used herein are for the purpose of facilitating use of reference only and shall not be construed to infer a contractual construction of language.
1. Section 1 shall be amended by deleting and replacing the following definitions:
Back-up Plan – A written plan that is a required component of the plan of care for all CHOICES members receiving companion care or non-residential CHOICES HCBS in their own home and which specifies unpaid persons as well as paid consumer-directed workers and/or contract providers (as applicable) who are available, have agreed to serve as back-up, and who will be contacted to deliver needed care in situations when regularly scheduled CHOICES HCBS providers or workers are unavailable or do not arrive as scheduled. A CHOICES member or his/her representative may not elect, as part of the back-up plan, to go without services. The backup plan shall include the names and telephone numbers of persons and agencies to contact and the services to be provided by each of the listed contacts. The member and his/her representative (as applicable) shall have primary responsibility for the development and implementation of the back-up plan for consumer directed services with assistance from the FEA as needed.
Care Coordination Team – If an MCO elects to use a care coordination team, the care coordination team shall consist of a care coordinator and specific other persons with relevant expertise and experience who are assigned to support the care coordinator in the performance of care coordination activities for a CHOICES member as specified in this Agreement and in accordance with Section 2.9.6., but shall not perform activities that must be performed by the Care Coordinator, including needs assessment, development of the plan of care, and minimum Care Coordination contacts.
Caregiver – For purposes of CHOICES, a person who is (a) a family member or is unrelated to the member but has a close, personal relationship with the member and (b) routinely involved in providing unpaid support and assistance to the member. A caregiver may be also designated by the member as a representative for CHOICES or for consumer direction of eligible CHOICES HCBS.
CHOICES Group (Group) – One of the three groups of TennCare enrollees who are enrolled in CHOICES. There are three CHOICES groups:
1. Group 1
Medicaid enrollees of all ages who are receiving Medicaid-reimbursed care in a nursing facility.
2. Group 2
Persons age sixty-five (65) and older and adults age twenty-one (21) and older with physical disabilities who meet the nursing facility level of care, who qualify for TennCare either as SSI recipients or as members of the CHOICES 217-Like HCBS Group, and who need and are receiving CHOICES HCBS as an alternative to nursing facility care. The CHOICES 217-Like HCBS Group includes persons who could have been eligible under 42 CFR 435.217 had the state continued its 1915(c) HCBS waiver for elders and/or persons with physical disabilities. TENNCARE has the discretion to apply an enrollment target to this group, as described in TennCare rules and regulations.
3. Group 3
Persons age sixty-five (65) and older and adults age twenty-one (21) and older with physical disabilities who qualify for TennCare as SSI recipients, who do not meet the nursing facility level of care, but who, in the absence of CHOICES HCBS, are “at-risk” for nursing facility care, as defined by the State. TENNCARE has the discretion to apply an enrollment target to this group, as described in TennCare rules and regulations. Group 3 was not included in CHOICES on the date of CHOICES implementation. TENNCARE intends to include CHOICES Group 3 at such time that the State is permitted to modify nursing facility level of care based on CMS interpretation of maintenance of effort requirements set forth in the Affordable Care Act. . TENNCARE will notify the CONTRACTOR at least sixty (60) days prior to the proposed date for including Group 3 in CHOICES. As of the date specified in that notice, the CONTRACTOR shall accept members in CHOICES Group 3 and shall implement all of the requirements in this Agreement that are applicable to CHOICES Group 3.
Consumer – Except when used regarding consumer direction of eligible CHOICES HCBS, an individual who uses a mental health or substance abuse service.
Consumer-Directed Worker (Worker) – An individual who has been hired by a CHOICES member participating in consumer direction of eligible CHOICES HCBS or his/her representative to provide one or more eligible CHOICES HCBS to the member. Worker does not include an employee of an agency that is being paid by an MCO to provide HCBS to the member.
Consumer Direction of Eligible CHOICES HCBS – The opportunity for a CHOICES member assessed to need specified types of CHOICES HCBS including attendant care, personal care, homemaker, in-home respite, companion care and/or any other service specified in TennCare rules and regulations as available for consumer direction to elect to direct and manage (or to have a representative direct and manage) certain aspects of the provision of such services—primarily, the hiring, firing, and day-to-day supervision of consumer-directed workers delivering the needed service(s).
Cost Neutrality Cap – The requirement that the cost of providing care to a member in CHOICES Group 2, including CHOICES HCBS and Medicaid reimbursed home health and private duty nursing, shall not exceed the cost of providing nursing facility services to the member, as determined in accordance with TennCare policy. A member’s individual cost neutrality cap shall be the average cost of Level 1 nursing facility care unless a higher cost neutrality cap is established by TennCare based on information submitted by the AAAD or MCO (as applicable) in the PAE application.
Disenrollment – The removal of an enrollee from participation in the CONTRACTOR’s MCO and deletion from the outbound 834 enrollment file furnished by TENNCARE to the CONTRACTOR.
Electronic Visit Verification (EVV) System – An electronic system into which provider staff and consumer-directed workers can check-in at the beginning and check-out at the end of each period of service delivery to monitor member receipt of specified CHOICES HCBS and which may also be utilized for submission of claims.
Eligible CHOICES HCBS – Attendant care, personal care, homemaker, in-home respite, companion care services and/or any other CHOICES HCBS specified in TennCare rules and regulations as eligible for consumer direction for which a CHOICES member is determined to need and elects to direct and manage (or have a representative direct and manage) certain aspects of the provision of such services – primarily the hiring, firing and day-to-day supervision of consumer-directed workers delivering the needed service(s). Eligible CHOICES HCBS do not include home health or private duty nursing services.
Employer of Record – The member participating in consumer direction of eligible CHOICES HCBS or a representative designated by the member to assume the consumer direction of eligible CHOICES HCBS functions on the member’s behalf.
Expenditure Cap – The annual limit on expenditures for CHOICES HCBS, excluding home modifications, for CHOICES members in CHOICES Group 3. The expenditure cap is $15,000.
Fiscal Employer Agent (FEA) – An entity contracting with the State and/or an MCO that helps CHOICES members participating in consumer direction of eligible CHOICES HCBS. The FEA provides both financial administration and supports brokerage functions for CHOICES members participating in consumer direction of eligible CHOICES HCBS. This term is used by the IRS to designate an entity operating under Section 3504 of the IRS code, Revenue Procedure 70-6 and Notice 2003-70, as the agent to members for the purpose of filing certain federal tax forms and paying federal income tax withholding, FICA and FUTA taxes. The FEA also files state income tax withholding and unemployment insurance tax forms and pays the associated taxes and processes payroll based on the eligible CHOICES HCBS authorized and provided.
Home and Community-Based Services (HCBS) – Services that are provided pursuant to a Section 1915(c) waiver or the CHOICES program as an alternative to long-term care institutional services in a nursing facility or an Intermediate Care Facility for the Mentally Retarded (ICF/MR). HCBS may also include optional or mandatory services that are covered by Tennessee’s Title XIX state plan or under the TennCare demonstration for all eligible enrollees, including home health or private duty nursing. However, only CHOICES HCBS are eligible for Consumer Direction. CHOICES HCBS do not include home health or private duty nursing services or any other HCBS that are covered by Tennessee’s Title XIX state plan or under the TennCare demonstration for all eligible enrollees, although such services are subject to estate recovery and shall be counted for purposes of determining whether a CHOICES member’s needs can be safely met in the community within his or her individual cost neutrality cap.
Immediate Eligibility – A mechanism by which the State can, based on a preliminary determination of a person’s eligibility for the CHOICES 217-Like HCBS Group, enroll the person into CHOICES Group 2 and provide immediate access to a limited package of CHOICES HCBS pending a final determination of eligibility. To qualify for immediate eligibility, a person must be applying to receive covered ongoing CHOICES HCBS, be determined by TENNCARE to meet nursing facility level of care, have submitted an application for financial eligibility determination to DHS, and be expected to qualify for CHOICES Group 2 based on review of the financial information provided by the applicant. Immediate eligibility shall only be for specified CHOICES HCBS (no other covered services) and for a maximum of forty-five (45) days from the effective date of eligibility.
One-Time CHOICES HCBS – Specified CHOICES HCBS which occur as a distinct event or which may be episodic in nature (occurring at less frequent irregular intervals or on an as needed basis for a limited duration of time). One-time HCBS include in-home respite, in-patient respite, assistive technology, minor home modifications, and/or pest control.
Ongoing CHOICES HCBS – Specified CHOICES HCBS which are delivered on a regular and ongoing basis, generally one or more times each week, or (in the case of community-based residential alternatives and PERS) on a continuous basis. Ongoing HCBS include community- based residential alternatives, personal care, attendant care, homemaker services, home-delivered meals, personal emergency response systems (PERS), and/or adult day care.
Representative – In general, for CHOICES members, a person who is at least eighteen (18) years of age and is authorized by the member to participate in care planning and implementation and to speak and make decisions on the member’s behalf, including but not limited to identification of needs, preference regarding services and service delivery settings, and communication and resolution of complaints and concerns. As it relates to consumer direction of eligible CHOICES HCBS, a person who is authorized by the member to direct and manage the member’s worker(s), and signs a representative agreement. The representative for consumer direction of eligible CHOICES HCBS must also: be at least eighteen (18) years of age; have a personal relationship with the member and understand his/her support needs; know the member’s daily schedule and routine, medical and functional status, medication regimen, likes and dislikes, and strengths and weaknesses; and be physically present in the member’s residence on a regular basis or at least at a frequency necessary to supervise and evaluate workers.
Representative Agreement – The agreement between a CHOICES member electing consumer direction of eligible CHOICES HCBS who has a representative direct and manage the consumer’s worker(s) and the member’s representative that specifies the roles and responsibilities of the member and the member’s representative.
Risk Agreement – An agreement signed by a member who will receive CHOICES HCBS (or his/her representative) that includes, at a minimum, identified risks to the member of residing in the community and receiving HCBS, the possible consequences of such risks, strategies to mitigate the identified risks, and the member’s decision regarding his/her acceptance of risk. For members electing to participate in consumer direction, the risk agreement must include any additional risks associated with the member’s decision to act as the employer of record, or to have a representative act as the employer of record on his/her behalf. See Section 2.9.6 of this Agreement for related requirements.
Self-Direction of Health Care Tasks – A decision by a CHOICES member participating
in
consumer direction to direct and supervise a paid worker delivering eligible CHOICES HCBS in
the performance of health care tasks that would otherwise be performed by a licensed nurse.
Self- direction of health care tasks is not a service, but rather health care-related duties
and functions (such as administration of medications) that a CHOICES member participating in
consumer direction may elect to have performed by a consumer-directed worker as part of the
delivery of eligible CHOICES HCBS s/he is authorized to receive.
Service Agreement – The agreement between a CHOICES member electing consumer direction of eligible CHOICES HCBS (or the member’s representative) and the member’s consumer- directed worker that specifies the roles and responsibilities of the member (or the member’s representative) and the member’s worker.
Service Gap – A delay in initiating any long-term care service and/or a disruption of a scheduled, ongoing CHOICES HCBS that was not initiated by a member, including late and missed visits.
Supports Broker – An individual assigned by the FEA to each CHOICES member participating in consumer direction who assists the member/representative in performing the employer of record functions, including, but not limited to: developing job descriptions; locating; recruiting; interviewing; scheduling; monitoring; and evaluating workers. The supports broker collaborates with, but does not duplicate, the functions of the member’s care coordinator. The supports broker does not have authority or responsibility for consumer direction. The member or member’s representative must retain authority and responsibility for consumer direction.
| 2. | Section 1 shall be amended by adding the following definition: |
CHOICES Home and Community-Based Services (HCBS) – Services that are available only to eligible persons enrolled in CHOICES Group 2 or Group 3 as an alternative to long-term care institutional services in a nursing facility or to delay or prevent placement in a nursing facility. Only CHOICES HCBS are eligible for Consumer Direction. CHOICES HCBS do not include home health or private duty nursing services or any other HCBS that are covered by Tennessee’s Title XIX state plan or under the TennCare demonstration for all eligible enrollees, although such services are subject to estate recovery and shall be counted for purposes of determining whether a CHOICES member’s needs can be safely met in the community within his or her individual cost neutrality cap.
| 3. | Sections 2.4.5.1 and 2.4.5.2 shall be amended by adding the words “outbound 834” in front of the words “enrollment file”. |
| 4. | Section 2.4.6.1 shall be amended by adding the words “outbound 834” in front of the words “enrollment files”. |
| 5. | Section 2.4.6.2 shall be amended by adding the words “(inbound 834)” after the words “eligibility file”. |
| 6. | The first sentence of the third paragraph in the Benefit Limit description for “Non-Emergency Medical Transportation (Including Non-Emergency Ambulance Transportation)” of Section 2.6.1.3 shall be amended by deleting the phrase “, including services”. |
“The CONTRACTOR is not responsible for providing NEMT to HCBS provided through a 19 15(c) waiver program for persons with intellectual disabilities (i.e., mental retardation) and HCBS provided through the CHOICES program.”
| 7. | Sections 2.6.1.5 through 2.6.1.5.8.5 shall be deleted and replaced as follows: |
2.6.1.5 Long-Term Care Benefits for CHOICES Members
| 2.6.1.5.1 | In addition to physical health benefits (see Section 2.6.1.3) and behavioral health benefits (see Section 2.6.1.4), the CONTRACTOR shall provide long-term care services (including CHOICES HCBS and nursing facility care) as described in this Section 2.6.1.5 to members who have been enrolled into CHOICES by TENNCARE, as shown in the outbound 834 enrollment file furnished by TENNCARE to the CONTRACTOR, effective upon the CHOICES Implementation Date (see Section 1). |
| 2.6.1.5.2 | TennCare enrollees will be enrolled by TENNCARE into CHOICES if the following conditions, at a minimum, are met: |
| 2.6.1.5.2.1 | TENNCARE or its designee determines the enrollee meets the categorical and financial eligibility criteria for Group 1, 2 or 3; |
| 2.6.1.5.2.2 | For Groups 1 and 2, TENNCARE determines that the enrollee meets nursing facility level of care including for Group 2, that the enrollee needs ongoing CHOICES HCBS in order to live safely in the home or community setting and to delay or prevent nursing facility placement; |
| 2.6.1.5.2.3 | For Group 2, the CONTRACTOR or, for new TennCare applicants, TENNCARE or its designee, determines that the enrollee’s combined CHOICES HCBS, private duty nursing and home health care can be safely provided at a cost less than the cost of nursing facility care for the member; |
| 2.6.1.5.2.4 | For Group 3, TENNCARE determines that the enrollee meets the at-risk level of care; and |
| 2.6.1.5.2.5 | For Groups 2 and 3, if there is an enrollment target, TENNCARE determines that the enrollment target has not been met or, for Group 2, approves the CONTRACTOR’s request to provide CHOICES HCBS as a cost effective alternative (see Section 2.6.5). Enrollees transitioning from a nursing facility to the community will not be subject to the enrollment target for Group 2 but must meet categorical and financial eligibility for Group 2. |
| 2.6.1.5.3 | For persons determined to be eligible for enrollment in Group 2 as a result of Immediate Eligibility (as defined in Section 1 of this Agreement), the CONTRACTOR shall provide a limited package of CHOICES HCBS (personal care, attendant care, homemaker services, home-delivered meals, PERS, adult day care, and/or any other services as specified in TennCare rules and regulations) as identified through a needs assessment and specified in the plan of care. Upon notice that the State has determined that the member meets categorical and financial eligibility for TennCare CHOICES, the CONTRACTOR shall authorize additional services in accordance with Section 2.9.6.2.5. For members residing in a community-based residential alternative at the time of CHOICES enrollment, authorization for community- based residential alternative services shall be retroactive to the member’s effective date of CHOICES enrollment. |
| 2.6.1.5.4 | The following long-term care services are available to CHOICES members, per Group, when the services have been determined medically necessary by the CONTRACTOR. |
| Service and Benefit Limit | Group 1 | Group 2 | Group 3 | |||
Nursing facility care
|
X | Short-term only (up to 90 days) |
Short-term only (up to 90 days) |
|||
Community-based residential alternatives |
X |
|||||
Personal care visits (up to 2 visits per day) |
X |
X |
||||
Attendant care (up to 1080 hours per calendar year) |
X |
X |
||||
Homemaker services (up to 3 visits per week) |
X |
X |
||||
Home-delivered meals (up to 1 meal per day) |
X |
X |
||||
Personal Emergency Response Systems (PERS) |
X |
X |
||||
Adult day care (up to 2080 hours per calendar year) |
X |
X |
||||
In-home respite care (up to 216 hours per calendar year) |
X |
X |
||||
In-patient respite care (up to 9 days per calendar year) |
X |
X |
||||
Assistive technology (up to $900 per calendar year) |
X |
X |
||||
Minor home modifications (up to $6,000 per project; $10,000 per calendar year; and $20,000 per lifetime) |
X |
X |
||||
Pest control (up to 9 units per calendar year) |
X |
X |
||||
| 2.6.1.5.5 | In addition to the benefit limits described above, in no case shall the CONTRACTOR exceed the member’s individual cost neutrality cap (as defined in Section 1 of this Agreement) for CHOICES Group 2 or the expenditure cap for Group 3. |
| 2.6.1.5.5.1 | For CHOICES members in Group 2, the services that shall be compared against the member’s individual cost neutrality cap include the total cost of CHOICES HCBS and Medicaid reimbursed home health care and private duty nursing. The total cost of CHOICES HCBS includes all covered CHOICES HCBS and other non-covered services that the CONTRACTOR elects to offer as a cost effective alternative to nursing facility care pursuant to Section 2.6.5.2 of this Agreement including, as applicable: CHOICES HCBS in excess of specified CHOICES benefit limits, the one-time transition allowance for Group 2 and NEMT for Groups 2 and 3. |
| 2.6.1.5.5.1 | For CHOICES members in Group 3, the total cost of CHOICES HCBS, excluding minor home modifications, shall not exceed the expenditure cap (as defined in Section 1 of this Agreement). |
| 2.6.1.5.6 | CHOICES members may, pursuant to Section 2.9.7, choose to participate in consumer direction of eligible CHOICES HCBS and, at a minimum, hire, fire and supervise workers of eligible CHOICES HCBS. |
| 2.6.1.5.7 | The CONTRACTOR shall, on an ongoing basis, monitor CHOICES members’ receipt and utilization of long-term care services and identify CHOICES members who are not receiving long-term care services. Pursuant to Section 2.30.10.5, the CONTRACTOR shall, on a monthly basis, notify TENNCARE regarding members that have not received long-term care services for a thirty (30) day period of time. The CONTRACTOR shall be responsible for immediately initiating disenrollment of any member who is not receiving TennCare reimbursed long-term care services and is not expected to resume receiving long-term care services within the next thirty (30) days, except under extenuating circumstances which must be reported to TennCare on the CHOICES Utilization Report. Acceptable circumstances may include, but are not limited to, a member’s temporary hospitalization or temporary receipt of Medicare-reimbursed skilled nursing facility care. Such notification and/or disenrollment shall be based not only on receipt and/or payment of claims for long-term care services, but also upon review and investigation by the CONTRACTOR as needed to determine whether the member has received long-term care services, regardless of whether claims for such services have been submitted or paid. |
| 2.6.1.5.8 | The CONTRACTOR may submit to TENNCARE a request to no longer provide long-term care services to a member due to concerns regarding the ability to safely and effectively care for the member in the community and/or to ensure the member’s health, safety and welfare. Acceptable reasons for this request include but are not limited to the following: |
| 2.6.1.5.8.1 | A member in Group 2 for whom the CONTRACTOR has determined that it cannot safely and effectively meet the member’s needs at a cost that is less than the member’ cost neutrality cap, and the member declines to transition to a nursing facility; |
| 2.6.1.5.8.2 | A member in Group 2 or 3 who repeatedly refuses to allow a care coordinator entrance into his/her place of residence (Section 2.9.6); |
| 2.6.1.5.8.3 | A member in Group 2 or 3 who refuses to receive critical HCBS as identified through a needs assessment and documented in the member’s plan of care; and |
| 2.6.1.5.8.4 | A member in Group 1 who fails to pay his/her patient liability and the CONTRACTOR is unable to find a nursing facility willing to provide services to the member (Section 2.6.7.2). |
| 2.6.1.5.8.5 | A member in Group 2 or 3 who refuses to pay his/her patient liability and for whom the CONTRACTOR is either: 1) in the case of persons receiving CBRA services, unable to identify another provider willing to provide services to the member; or 2) in the case of persons receiving non-residential HCBS or companion care, the CONTRACTOR is unwilling to continue to serve the member, and the Bureau of TennCare has determined that no other MCO is willing to serve the member. |
| 2.6.1.5.8.6 | The CONTRACTOR’s request to no longer provide long-term care services to a member shall include documentation as specified by TENNCARE. The State shall make any and all determinations regarding whether the CONTRACTOR may discontinue providing long-term care services to a member, disenrollment from CHOICES, and, as applicable, termination from TennCare. |
| 2.6.1.5.9 | The CONTRACTOR may submit to TENNCARE a request to disenroll from CHOICES a member who is not receiving any Medicaid-reimbursed LTC services based on the CONTRACTOR’s inability to reach the member only when the CONTRACTOR has exhausted all reasonable efforts to contact the member, and has documented such efforts in writing, which must be submitted with the disenrollment request. Efforts to contact the member shall include, at a minimum: |
| 2.6.1.5.9.1 | Multiple attempts to contact the member, his/her representative or designee (as applicable) by phone. Such attempts must occur over a period of at least two (2) weeks and at different times of the day and evening, including after business hours. The CONTRACTOR shall attempt to contact the member at the phone number provided in the outbound 834 enrollment file, any additional phone numbers the CONTRACTOR has on file, including referral records and case management notes; and phone numbers that may be provided in TENNCARE’s TPAES system. The CONTRACTOR shall also contact the member’s Primary Care Provider and any contracted LTC providers that have delivered services to the member during the previous six (6) months in order to obtain contact information that can be used to reach the member; |
| 2.6.1.5.9.2 | At least one (1) visit to the member’s most recently reported place of residence except in circumstances where significant safety concerns prevent the CONTRACTOR from completing the visit, which shall be documented in writing; and |
| 2.6.1.5.9.3 | An attempt to contact the member by mail at the member’s most recently reported place of residence at least two (2) weeks prior to the request to disenroll. |
| 8. | Sections 2.6.5.2.1 through 2.6.5.2.3 shall be amended by inserting the word “CHOICES” before the word “HCBS”. |
9. Section 2.6.5.3 shall be deleted and replaced as follows:
| 2.6.5.3 | If the CONTRACTOR chooses to provide cost effective alternative services to a CHOICES member, in no case shall the cost of CHOICES HCBS, private duty nursing and home health care for Group 2 exceed a member’s cost neutrality cap nor the total cost of CHOICES HCBS, excluding minor home modifications, for members in Group 3 exceed the expenditure cap. The total cost of CHOICES HCBS includes all covered CHOICES HCBS and other non-covered services that the CONTRACTOR elects to offer as a cost effective alternative to nursing facility care pursuant to Section 2.6.5.2 of this Agreement including, as applicable: CHOICES HCBS in excess of specified benefit limits, the one-time transition allowance for Group 2 and NEMT for Groups 2 and 3. |
10. Sections 2.6.7.2 through 2.6.7.2.5 shall be deleted and replaced as follows:
| 2.6.7.2 | Patient Liability |
| 2.6.7.2.1 | TENNCARE will notify the CONTRACTOR of any applicable patient liability amounts for CHOICES members via the outbound 834 enrollment file. |
| 2.6.7.2.1.1 | When TENNCARE notifies the CONTRACTOR of patient liability amounts for CHOICES members via the outbound 834 enrollment file with an effective date any time other than the first day of the month, the CONTRACTOR shall determine and apply the pro-rated portion of patient liability for that month. |
| 2.6.7.2.2 | The CONTRACTOR shall delegate collection of patient liability for CHOICES Group 1 members to the nursing facility and shall pay the facility net of the applicable patient liability amount. |
| 2.6.7.2.2.1 | In accordance with the involuntary discharge process, including notice and appeal (see Section 2.12.11.3), a nursing facility may refuse to continue providing services to a member who fails to pay his or her patient liability and for whom the nursing facility can demonstrate to the CONTRACTOR that it has made a good faith effort to collect payment. |
| 2.6.7.2.2.2 | If the CONTRACTOR is notified that a nursing facility is considering discharging a member (see Section 2.12.11.3), the CONTRACTOR shall work to find an alternate nursing facility willing to serve the member and document its efforts in the member’s files. |
| 2.6.7.2.2.3 | If the CONTRACTOR is unable to find an alternate nursing facility willing to serve the member and the member otherwise qualifies to enroll in CHOICES Group 2, the CONTRACTOR shall determine if it can safely and effectively serve the member in the community and within the cost neutrality cap. If it can, and the CONTRACTOR is willing to continue serving a member who has failed to pay his or her patient liability or if TENNCARE determines that the member would not have patient liability in the community setting, the member shall be offered a choice of CHOICES HCBS. If the member chooses CHOICES HCBS, the CONTRACTOR shall forward all relevant information to TENNCARE for a decision regarding transition to Group 2 (Section 2.9.6.3). |
| 2.6.7.2.2.4 | If the CONTRACTOR is unable to find an alternate nursing facility willing to serve the member and the CONTRACTOR determines that it cannot safely and effectively serve the member in the community and within the cost neutrality cap, the member declines to enroll in Group 2, or TENNCARE determines that the member would continue to have patient liability in the community setting and the CONTRACTOR is unwilling to continue serving the member who has failed to pay his or her patient liability, or TENNCARE denies enrollment in Group 2, the CONTRACTOR may, pursuant to Section 2.6.1.5.8, request to no longer provide long-term care services to the member. |
| 2.6.7.2.3 | For CHOICES Group 2 and 3 members, patient liability shall be collected as follows: |
| 2.6.7.2.3.1 | The CONTRACTOR shall delegate collection of patient liability for CHOICES Group 2 members who reside in a CBRA facility to the CBRA facility and shall pay the facility net of the applicable patient liability amount. |
| 2.6.7.2.3.2 | The CONTRACTOR shall collect patient liability from CHOICES Group 2 and Group 3 members (as applicable) who receive CHOICES HCBS in his/her own home and from Group 2 members who receive Companion Care. |
| 2.6.7.2.3.2.1 | The CONTRACTOR shall use calculated patient liability amounts to offset the cost of CHOICES Group 2 benefits (or CEA services provided as an alternative to covered CHOICES Group 2 benefits) reimbursed by the CONTRACTOR for that month. |
| 2.6.7.2.3.2.2 | The CONTRACTOR shall not collect patient liability that exceeds the cost of CHOICES Group 2 benefits (or CEA services provided as an alternative to CHOICES Group 2 benefits) reimbursed by the CONTRACTOR for that month. |
| 2.6.7.2.3.2.3 | The CONTRACTOR shall, upon notification in the outbound 834 enrollment file of retroactive adjustments in patient liability amounts based on Item D deductions, without requiring any action on the part of the member or provider, adjust the Group 2 or Group 3 member’s patient liability for the following month(s) until reimbursement of any overpayment is accomplished, or shall refund any overpayments within thirty (30) days of a request from the member or when the member will not continue to have patient liability obligations going forward. |
| 2.6.7.2.3.3 | If a Group 2 member fails to pay required patient liability, pursuant to Section 2.6.1.5.8.5, the CONTRACTOR may request to no longer provide long-term care services to the member. |
| 2.6.7.2.3.4 | The CONTRACTOR shall not waive or otherwise fail to establish and maintain processes for collection of patient liability in accordance with this Agreement. |
11. Section 2.7.2.1.2 shall be deleted and replaced as follows:
| 2.7.2.1.2 | The CONTRACTOR shall provide behavioral health services in accordance with this Agreement, TennCare Rules and Regulations and TennCare policies, including Section 2.6 and Attachment I of this Agreement, and TennCare Medical Necessity Rule 1200-13- 16. |
12. Section 2.7.3 shall be deleted and replaced as follows:
| 2.7.3 | Self-Direction of Health Care Tasks |
The CONTRACTOR shall, in accordance with TennCare rules and regulations, permit CHOICES members the option to direct and supervise a consumer-directed worker who is providing eligible CHOICES HCBS in the performance of health care tasks.
| 13. | Section 2.8.1.2 shall be amended by adding the phrase updated as described in current NCQA Standards” as follows: |
| 2.8.1.2 | Each DM program shall utilize evidence-based clinical practice guidelines (hereafter referred to as the guidelines) that have been formally adopted and updated as described in current NCQA Standards by the CONTRACTOR’s Quality Management/Quality Improvement (QM/QI) committee or other clinical committee as a clinical basis for development of program content and plan of care. |
14. Section 2.8.1.6 shall be deleted and replaced as follows:
| 2.8.1.6 | As part of its DM program descriptions, the CONTRACTOR shall also describe how the organization integrates member information and coordinates with and has timely access to MCO case management activities and other supporting entities, including but not limited to, Utilization Management (UM), CHOICES, Health Information Lines and Wellness programs, to assure programs are linked and enrollees receive appropriate and timely care. |
15. Section 2.8.7.2 shall be amended by deleting the word “passive”.
| 2.8.7.2 | The CONRACTOR shall report the participation rates (as defined by NCQA) and the number of individuals participating in each level of each of the DM programs. |
16. Sections 2.9.2.1.4 through 2.9.2.1.4.6.5 shall be deleted and replaced as follows:
| 2.9.2.1.4 | For covered long-term care services for CHOICES members who are transferring from another MCO, the CONTRACTOR shall be responsible for continuing to provide covered long-term care services, including both CHOICES HCBS authorized by the transferring MCO and nursing facility services, without regard to whether such services are being provided by contract or non-contract providers. |
| 2.9.2.1.4.1 | For a member in CHOICES Group 2 or 3, the CONTRACTOR shall continue CHOICES HCBS authorized by the transferring MCO for a minimum of thirty (30) days after the member’s enrollment and thereafter shall not reduce these services unless a care coordinator has conducted a comprehensive needs assessment and developed a plan of care, and the CONTRACTOR has authorized and initiated CHOICES HCBS in accordance with the member’s new plan of care. If a member in CHOICES Group 2 or 3 is receiving short-term nursing facility care, the CONTRACTOR shall continue to provide nursing facility services to the member in accordance with the level of nursing facility services (Level I or Level II) and/or reimbursement approved by TENNCARE (see Section 2.14.1.12). For a member in Group 1, the CONTRACTOR shall provide nursing facility services to the member in accordance with the level of nursing facility services (Level I or Level II) and/or reimbursement approved by TENNCARE (see Section 2.14.1.12); however, the member may be transitioned to the community in accordance with Section 2.9.6.8 of this Agreement. |
| 2.9.2.1.4.2 | For a member in CHOICES Group 2 or 3, within thirty (30) days of notice of the member’s enrollment with the CONTRACTOR, a care coordinator shall conduct a face- to-face visit (see Section 2.9.6.2.5), including a comprehensive needs assessment (see Section 2.9.6.5), and develop a plan of care (see Section 2.9.6.6), and the CONTRACTOR shall authorize and initiate CHOICES HCBS in accordance with the new plan of care (see Section 2.9.6.2.5). If a member in Group 2 or 3 is receiving short- term nursing facility care on the date of enrollment with the CONTRACTOR, a care coordinator shall complete a face-to-face visit prior to the expiration date of the level of nursing facility services approved by TENNCARE, but no later than thirty (30) days after enrollment to determine appropriate needs assessment and care planning activities (see Section 2.9.6.2.5 for members who will be discharged from the nursing facility and remain in Group 2 or 3 and Section 2.9.6.2.4 for members who will remain in the nursing facility and be enrolled in Group 1). If the expiration date for the level of nursing facility services approved by TENNCARE occurs prior to thirty (30) days after enrollment, and the CONTRACTOR is unable to conduct the face-to-face visit prior to the expiration date, the CONTRACTOR shall be responsible for facilitating discharge to the community or enrollment in Group 1, whichever is appropriate prior to the member’s exhaustion of the 90-day short-term NF benefit. |
| 2.9.2.1.4.3 | If at any time before conducting a comprehensive needs assessment for a member in CHOICES Group 2 or 3 the CONTRACTOR becomes aware of an increase in the member’s needs, a care coordinator shall immediately conduct a comprehensive needs assessment and update the member’s plan of care, and the CONTRACTOR shall initiate the change in services within ten (10) days of becoming aware of the increase in the member’s needs. |
| 2.9.2.1.4.4 | For a member in CHOICES Group 1, a care coordinator shall conduct a face-to-face in- facility visit within thirty (30) days of the member’s enrollment with the CONTRACTOR and conduct a needs assessment as determined necessary by the CONTRACTOR (see Section 2.9.6.5). |
| 2.9.2.1.4.5 | The CONTRACTOR shall facilitate a seamless transition to new services and/or providers, as applicable, in the plan of care developed by the CONTRACTOR without any disruption in services. |
| 2.9.2.1.4.6 | The CONTRACTOR shall not: |
| 2.9.2.1.4.6.1 | Transition nursing facility residents or residents of community-based residential alternatives to another facility unless (1) the member or his/her representative specifically requests to transition, which shall be documented in the member’s file, (2) the member or his/her representative provides written consent to transition based on quality or other concerns raised by the CONTRACTOR, which shall not include the nursing facility’s rate of reimbursement; or (3) the facility where the member is residing is not a contract provider; if the community-based residential facility where the member is currently residing is not a contract provider, the CONTRACTOR shall provide continuation of services in such facility for at least thirty (30) days, which shall be extended as necessary to ensure continuity of care pending the facility’s contracting with the CONTRACTOR or the member’s transition to a contract facility; if the member is transitioned to a contract facility, the CONTRACTOR shall facilitate a seamless transition to the new facility; if the nursing facility where the member is currently residing is a non-contract provider, the CONTRACTOR shall (a) authorize continuation of the services pending enrollment of the facility as a contract provider (except a facility excluded for a 2-year period when the facility has withdrawn from Medicaid participation); (b) authorize continuation of the services pending facilitation of the member’s transition to a contract facility, subject to the member’s agreement with such transition; or (c) may continue to reimburse services from the non-contract nursing facility in accordance with TennCare rules and regulations; |
| 2.9.2.1.4.6.2 | Transition Group 1 members to CHOICES HCBS unless the member chooses to receive CHOICES HCBS as an alternative to nursing facility care and is enrolled in CHOICES Group 2 (see Section 2.9.6.8 for requirements regarding nursing facility to community transition); |
| 2.9.2.1.4.6.3 | Admit a member in CHOICES Group 2 to a nursing facility unless (1) the member requires a short-term nursing facility care stay; (2) the member chooses to transition to a nursing facility and enroll in Group 1; or (3) the CONTRACTOR determines that it cannot safely and effectively meet the needs of the member and within the member’s cost neutrality cap, and the member agrees to transition to a nursing facility and enroll in Group 1; |
| 2.9.2.1.4.6.4 | Admit a member enrolled in CHOICES Group 3 to a nursing facility unless: (1) the member meets nursing facility level of care and is expected to require nursing facility services for ninety (90) days or less; or (2) the member meets nursing facility level of care, is expected to require nursing facility services for more than ninety (90) days and chooses to transition to a nursing facility and enroll in Group 1; or |
| 2.9.2.1.4.6.5 | Transition members in Group 2 or 3 to another HCBS provider for continuing services unless the current HCBS provider is not a contract provider; if the current HCBS provider is not a contract provider, the CONTRACTOR shall provide continuation of HCBS from that provider for at least thirty (30) days, which shall be extended as necessary to ensure continuity of care pending the provider’s contracting with the CONTRACTOR or the member’s transition to a contract provider; if the member is transitioned to a contract provider, the CONTRACTOR shall facilitate a seamless transition to the new provider. |
| 17. | Sections 2.9.2.1.5 through 2.9.2.1.5.6.4 shall be deleted in their entirety including any references thereto. |
| 18. | Section 2.9.2.5 shall be deleted and replaced as follows: |
| 2.9.2.5 | If the CONTRACTOR becomes aware that a CHOICES member will be transferring to another MCO, the CONTRACTOR (including, but not limited to the member’s care coordinator or care coordination team) shall, in accordance with protocols established by TENNCARE, work with the other MCO in facilitating a seamless transition for that member. |
19. Section 2.9.3.3, 2.9.3.4 and 2.9.3.6 shall be deleted and replaced as follows:
| 2.9.3.3 | For members in Group 2 the CONTRACTOR shall continue HCBS in the member’s approved HCBS E/D waiver plan of care except case management for a minimum of thirty (30) days after the member’s enrollment and thereafter shall not reduce HCBS unless the member’s care coordinator has conducted a comprehensive needs assessment and developed a plan of care and the CONTRACTOR has authorized and initiated HCBS in accordance with the member’s new plan of care. If a member in CHOICES Group 2 is receiving short-term nursing facility care, the CONTRACTOR shall continue to provide nursing facility services to the member in accordance with the level of nursing facility services (Level I or Level II) and/or reimbursement approved by TENNCARE (see Section 2.14.1.12). |
| 2.9.3.4 | For a member in CHOICES Group 2, within ninety (90) days of CHOICES implementation, the member’s care coordinator shall conduct a face-to-face visit (see Section 2.9.6.2.5), including a comprehensive needs assessment (see Section 2.9.6.5), and develop a plan of care (see Section 2.9.6.6), and the CONTRACTOR shall authorize and initiate CHOICES HCBS in accordance with the new plan of care. If a member in Group 2 is receiving short-term nursing facility care on the date of enrollment with the CONTRACTOR the member’s care coordinator shall complete a face-to-face visit prior to the expiration date of the level of nursing services approved by TENNCARE, but no more than ninety (90) days after CHOICES implementation, to determine appropriate needs assessment and care planning activities (see Section 2.9.6.2.5 for members who will be discharged from the nursing facility and remain in Group 2 or 3 and Section 2.9.6.2.4 for members who will remain in the nursing facility and be enrolled in Group 1). If the expiration date for the level of nursing facility services approved by TENNCARE occurs prior to ninety (90) days after CHOICES implementation, and the CONTRACTOR is unable to conduct the face-to-face visit prior to the expiration date, the CONTRACTOR shall be responsible for facilitating discharge to the community or enrollment in Group 1, whichever is appropriate. |
| 2.9.3.6 | The CONTRACTOR shall provide nursing facility services to a member in Group 1 in accordance with the level of nursing facility services (Level I or Level II) and/or reimbursement approved by TENNCARE (see Section 2.14.1.12); however, the member may be transitioned to the community in accordance with Section 2.9.6.8 of this Agreement. |
20. Section 2.9.3.9.2 and 2.9.3.9.4 shall be deleted and replaced as follows:
| 2.9.3.9.2 | Transition Group 1 members to CHOICES HCBS unless the member chooses to receive CHOICES HCBS as an alternative to nursing facility care and is enrolled in CHOICES Group 2 (see Section 2.9.6.8 for requirements regarding nursing facility to community transition); |
| 2.9.3.9.4 | Transition members in Group 2 or 3 to another HCBS provider for continuing services unless the current HCBS provider is not a contract provider; if the current HCBS provider is not a contract provider, the CONTRACTOR shall provide continuation of CHOICES HCBS from that provider for at least thirty (30) days, which shall be extended as necessary to ensure continuity of care pending the provider’s contracting with the CONTRACTOR or the member’s transition to a contract provider; if the member is transitioned to a contract provider, the CONTRACTOR shall facilitate a seamless transition to the new provider. |
| 21. | Section 2.9.6.1 shall be amended by adding a new Section 2.9.6.1.6 and renumbering the remaining Sections accordingly, including any references thereto. |
| 2.9.6.1.6 | The CONTRACTOR shall compute Care Coordination CHOICES-related timelines as follows; |
| 2.9.6.1.6.1 | The day of the initiating event (e.g., receipt of a referral or receipt of the outbound 834 enrollment file is not to be included in the computation; |
| 2.9.6.1.6.2 | The Calendar Day immediately following the initiating event is day one (1) of timelines utilizing calendar days. Each subsequent calendar day is included in the computation; and |
| 2.9.6.1.6.3 | The Business Day (see Section 1) immediately following the initiating event is day one (1) of timelines utilizing business days. Each subsequent business day is included in the computation. |
| 22. | Sections 2.9.6.2.3 through 2.9.6.2.3.8 shall be deleted and replaced as follows: |
2.9.6.2.3 Functions of the Single Point of Entry (SPOE)
| 2.9.6.2.3.1 | For persons wishing to apply for CHOICES, TENNCARE or its designee may employ a screening process, using the tools and protocols specified by TENNCARE, to assist with intake for persons new to both TennCare and CHOICES. Such screening process shall assess: (1) whether the applicant appears to meet categorical and financial eligibility criteria for CHOICES; (2) whether the applicant appears to meet nursing facility level of care; and (3) for applicants seeking access to CHOICES HCBS through enrollment in CHOICES Group 2, whether it appears that the applicant’s needs can be safely and effectively met in the community and at a cost that does not exceed nursing facility care. |
| 2.9.6.2.3.2 | For persons identified by TENNCARE or its designee as meeting the screening criteria, or for whom TENNCARE or its designee opts not to use a screening process, TENNCARE or its designee will conduct a face-to-face intake visit with the applicant. As part of this intake visit TENNCARE or its designee will, using the tools and protocols specified by TENNCARE, conduct a level of care and needs assessment; assess the member’s existing natural support system, including but not limited to informal supports provided by family and other caregivers, services that may be available at no cost to the member through other entities, and services that are reimbursable through other public or private funding sources, such as Medicare or long-term care insurance; and identify the long-term care services and home health and/or private duty nursing services that may be needed by the applicant upon enrollment into CHOICES that would build upon and not supplant a member’s existing natural support system. |
| 2.9.6.2.3.3 | TENNCARE or its designee shall conduct the intake visit, including the level of care and needs assessment, in the applicant’s place of residence, except under extenuating circumstances (such as the member’s hospitalization), which shall be documented in writing. |
| 2.9.6.2.3.4 | As part of the intake visit, TENNCARE or its designee shall: (1) provide general CHOICES education and information, as specified by TENNCARE, and assist in answering any questions the applicant may have; (2) provide information about estate recovery; (3) provide choice counseling and facilitate the selection of an MCO by the applicant or his/her representative; (4) provide information regarding freedom of choice of nursing facility versus CHOICES HCBS, both verbally and in writing, and obtain a Freedom of Choice form signed and dated by the applicant or his/her representative; (5) provide detailed information and obtain signed acknowledgement of understanding regarding a CHOICES member’s responsibility with respect to payment of patient liability amounts, including, as applicable, the potential consequences for non-payment of patient liability which may include loss of the member’s current nursing facility or CBRA provider or MCO, disenrollment from CHOICES, and to the extent the member’s eligibility is dependent on receipt of long-term care services, possible loss of eligibility for TennCare; and (6) for applicants who want to receive NF services, provide information regarding the completion of all PASRR requirements prior to nursing facility admission and conduct the level I PASRR screening; (7) for applicants who are seeking CHOICES HCBS: (a) conduct a risk assessment using a tool and protocol specified by TENNCARE and develop, as applicable, a risk agreement that shall be signed by the applicant or his/her representative and which shall include identified risks to the applicant, the consequences of such risks, strategies to mitigate the identified risks, and the applicant’s decision regarding his/her acceptance of risk; (b) make a determination regarding whether the applicant’s needs can be safely and effectively met in the community and at a cost that does not exceed nursing facility care, including explanation to the applicant regarding the individual cost neutrality cap, including that a change in a member’s needs or circumstances that would result in the cost neutrality cap being exceeded or that would result in the MCO’s inability to safely and effectively meet a member’s needs in the community and within the cost neutrality cap may result in the member’s disenrollment from CHOICES Group 2, in which case, the care coordinator will assist with transition to a more appropriate care delivery setting; and (c) provide information regarding consumer direction and obtain signed documentation of the applicant’s interest in participating in consumer direction; and (8) provide information regarding next steps in the process including the need for approval by TENNCARE to enroll in CHOICES and the functions of the CONTRACTOR, including that the CONTRACTOR will develop and approve a plan of care. |
| 2.9.6.2.3.5 | The listing of CHOICES HCBS and home health and/or private duty nursing services the member may need shall be used by TENNCARE or its designee to determine whether services can be provided within the member’s cost neutrality cap and may be further refined based on the CONTRACTOR’s comprehensive needs assessment and plan of care development processes. |
| 2.9.6.2.3.6 | The State will be responsible for determining TennCare categorical and financial eligibility and level of care and enrolling eligible TennCare members into CHOICES. |
| 2.9.6.2.3.7 | TENNCARE will notify the CONTRACTOR via the outbound 834 enrollment file when a person has been enrolled in CHOICES, the member’s CHOICES Group, and any applicable patient liability amounts (See Section 2.6.7). For members in CHOICES Group 2, TENNCARE will notify the CONTRACTOR of the member’s cost neutrality cap (see definition in Section 1 and Section 2.6.1.5.2.3), which shall be the average cost of Level 1 nursing facility care unless a higher cost neutrality cap is established by TENNCARE based on information submitted by the AAAD or MCO (as applicable) in the level of care. |
| 2.9.6.2.3.8 | TENNCARE or its designee will make available to the CONTRACTOR the documentation from the intake visit, including but not limited to the member’s level of care and needs assessment, the assessment of the member’s existing natural support system, the member’s risk assessment and signed risk agreement (for members in CHOICES Group 2), and the services identified by TENNCARE or its designee that the member may need upon CHOICES enrollment. |
23. Sections 2.9.6.2.4 through 2.9.6.2.4.8 shall be deleted and replaced as follows:
| 2.9.6.2.4 | Functions of the CONTRACTOR for Members in CHOICES Group 1 |
| 2.9.6.2.4.1 | For members enrolled in CHOICES Group 1, who are, upon CHOICES enrollment, receiving nursing facility services, the CONTRACTOR shall reimburse such services in accordance with the level of nursing facility services (Level I or Level II) and/or reimbursement approved by TENNCARE (see Section 2.14.1.12), except that the CONTRACTOR may reimburse a lesser level of service when such lesser level of service is billed by the facility. Reimbursement for such services shall be from the current provider as of the effective date of CHOICES enrollment. The CONTRACTOR shall not move members enrolled in CHOICES Group 1 who are, upon CHOICES enrollment, receiving nursing facility services, to another facility unless: (1) the member or his/her representative specifically requests to move, which shall be documented in the member’s file; (2) the member or his/her representative provides written consent to move based on quality or other concerns raised by the CONTRACTOR, which shall not include the nursing facility’s rate of reimbursement; or (3) the facility where the member is residing is not a contract provider. If the nursing facility is a non-contract provider, the CONTRACTOR shall (a) provide continuation of the services pending enrollment of the facility as a contract provider (except a facility excluded for a 2-year period when the facility has withdrawn from Medicaid participation); (b) provide continuation of the services pending facilitation of the member’s transition to a contract facility, subject to the member’s agreement with such transition; or (c) may continue to reimburse services from the non-contract nursing facility in accordance with TennCare rules and regulations. |
| 2.9.6.2.4.2 | The CONTRACTOR shall, within thirty (30) calendar days of notice of the member’s enrollment in CHOICES, conduct a face-to-face visit with the member and perform any additional needs assessment deemed necessary by the CONTRACTOR (see Section 2.9.6.5.1). The care coordinator shall review the plan of care developed by the nursing facility and may supplement the plan of care as necessary and appropriate (see Section 2.9.6.6.1). |
| 2.9.6.2.4.3 | The CONTRACTOR shall not transition members in Group 1 to CHOICES HCBS unless the member chooses to receive CHOICES HCBS as an alternative to nursing facility and is enrolled in Group 2. |
| 2.9.6.2.4.4 | For purposes of the CHOICES program, the CONTRACTOR may decide whether it will issue service authorizations for nursing facility services, or whether it will instead process claims for such services in accordance with the level of care and/or reimbursement (including the duration of such level of care and/or reimbursement) approved by TENNCARE (see Section 2.14.1.12), except that the CONTRACTOR may reimburse a lesser level of service when such lesser level of service is billed by the facility. . |
| 2.9.6.2.4.5 | For CHOICES members approved by TENNCARE for Level II (or skilled) nursing facility services, the CONTRACTOR shall be responsible for monitoring the member’s continued need for Medicaid reimbursed skilled and/or rehabilitation services, promptly notifying TENNCARE when Level II nursing facility services are no longer medically necessary, and for the submission of information needed by TENNCARE to reevaluate the member’s level of care for nursing facility services (see also Section 2.14.1.12.2). |
| 24. | Sections 2.9.6.2.5.2 and 2.9.6.2.5.3 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 25. | Sections 2.9.6.2.5.8 through 2.9.6.2.5.13 shall be deleted and replaced as follows: |
| 2.9.6.2.5.8 | As part of the face-to-face visit for members in CHOICES Group 2, the care coordinator shall review, and revise as necessary, the member’s risk assessment and risk agreement and have the member or his/her representative sign and date any revised risk agreement. |
| 2.9.6.2.5.9 | As part of the face-to-face visit, for members determined to need eligible CHOICES HCBS, the care coordinator shall verify the member’s interest in participating in consumer direction and obtain written confirmation of the member’s decision. The care coordinator shall also provide member education regarding choice of contract providers for CHOICES HCBS, subject to the provider’s availability and willingness to timely deliver services, and obtain signed confirmation of the member’s choice of contract providers. |
| 2.9.6.2.5.10 | For purposes of CHOICES HCBS, service authorizations shall include the amount, frequency, and duration of each service to be provided and the schedule at which such care is needed, as applicable; the requested start date; and other relevant information as prescribed by TENNCARE. The CONTRACTOR shall be responsible for confirming the provider’s capacity and commitment to initiate services as authorized on or before the requested start date, and if the provider is unable to initiate services as authorized on or before the requested start date, for arranging an alternative provider who is able to initiate services as authorized on or before the requested start date. |
| 2.9.6.2.5.11 | The member’s care coordinator/care coordination team shall provide at least verbal notification to the member prior to initiation of CHOICES HCBS identified in the plan of care regarding any change in providers selected by the member for each CHOICES HCBS, including the reason such change has been made. |
| 2.9.6.2.5.12 | If the CONTRACTOR is unable to initiate any CHOICES HCBS in accordance with the timeframes specified herein, the CONTRACTOR shall issue written notice to the member, documenting the service(s) that will be delayed, the reasons for the delay, and the date the service(s) will start, and shall make good faith efforts to ensure that services are provided as soon as practical. |
| 2.9.6.2.5.13 | TENNCARE may establish, pursuant to policies and protocols for management of waiting lists, alternative timeframes for completion of specified intake functions and activities when there is a waiting list. |
26. Section 2.9.6.3.1.5 through 2.9.6.3.1.5.5 shall be deleted and replaced as follows:
| 2.9.6.3.1.5Periodic review (at least quarterly) of: | ||
| 2.9.6.3.1.5.1 2.9.6.3.1.5.2 2.9.6.3.1.5.3 2.9.6.3.1.5.4 |
Claims or encounter data; Hospital admission or discharge data; Pharmacy data; and Data collected through the DM and/or UM processes. |
|
| 2.9.6.3.1.5.5 | The CONTRACTOR may define in its policies and procedures other steps that will be taken to better assess if the members identified through means other than referral or notice of hospital admission will likely qualify for CHOICES, and may target its screening and intake efforts to a more targeted list of persons that are most likely to need and to qualify for CHOICES services. |
| 2.9.6.3.1.5.6 | TENNCARE may establish, pursuant to policies and protocols for management of waiting lists, alternative timeframes for completion this task when there is a waiting list. |
27. Section 2.9.6.3.2 shall be deleted and replaced as follows:
| 2.9.6.3.2 | As part of its identification process for members who may be eligible for CHOICES, the CONTRACTOR may initiate a telephone screening process, using the tool and protocols specified by TENNCARE. Such screening process shall: (1) verify the member’s current eligibility category based on information provided by TENNCARE in the outbound 834 enrollment file; for persons seeking access to CHOICES HCBS through enrollment in CHOICES Groups 2 or 3, identify whether the member meets categorical eligibility requirements for enrollment in such group based on his/her current eligibility category, and if not, for persons seeking to enroll in CHOICES Group 2, whether the member appears to meet categorical and financial eligibility criteria for the Institutional (i.e., CHOICES 217-Like HCBS) category; (2) determine whether the member appears to meet level of care eligibility for CHOICES; and (3) for members seeking access to CHOICES HCBS through enrollment in CHOICES Group 2, determine whether it appears that the member’s needs can be safely and effectively met in the community and at a cost that does not exceed nursing facility care. Such telephone screening shall be conducted at the time of the initial call by the CONTRACTOR unless the member requests that the screening be conducted at another time, which shall be documented in writing in the CHOICES intake record. |
28. Section 2.9.6.3.3.1 shall be deleted and replaced as follows:
| 2.9.6.3.3.1 | Documentation of at least three (3) attempts occurring over a period of no less than three (3) days to contact the member by phone (which shall include at least one (1) attempt to contact the member at the number most recently reported by the member and at least one (1) attempt to contact the member at the number provided in the referral, if different, and which shall occur at different times of the day and evening, including after business hours), followed by a letter sent to the member’s most recently reported address that provides information about CHOICES and how to obtain a screening for CHOICES, shall constitute sufficient effort by the CONTRACTOR to assist a member who has been referred for CHOICES, regardless of referral source. TENNCARE will review the CONTRACTOR’s referral data, including the number of referred members the CONTRACTOR is unable to reach, and may institute additional requirements as necessary to ensure reasonable efforts to reach the member and complete the referral and intake process. |
| 29. | Section 2.9.6.3.7 shall be deleted and replaced as follows: |
| 2.9.6.3.7 | If the member does not meet the telephone screening criteria, the CONTRACTOR shall notify the member verbally and in writing in the format prescribed by TENNCARE: (1) that he/she does not appear to meet the criteria for enrollment in CHOICES; (2) that he/she has the right to continue with the CHOICES intake process and, if determined not eligible, to receive notice of such denial, including the member’s due process right to appeal; and (3) how, if the member wishes to proceed with the CHOICES intake process, the member can submit a written request to proceed with the CHOICES intake process to the CONTRACTOR. In the event that a member does submit such written request, the CONTRACTOR shall process the request as a new referral and shall conduct a face-to-face intake visit, including level of care assessment and needs assessment, within ten (10) business days of receipt of the member’s written request, unless a later date is requested by the member, which shall be documented in writing in the CHOICES intake record. |
| 30. | Section 2.9.6.3.8.2 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 31. | Sections 2.9.6.3.9 through 2.9.6.3.18 shall be deleted and replaced as follows: |
| 2.9.6.3.9 | As part of the face-to-face intake visit, the care coordinator shall: (1) provide general CHOICES education and information, as specified by TENNCARE, to the member and assist in answering questions the member may have; (2) provide information about estate recovery; (3) provide assistance, as necessary, in facilitating gathering of categorical/financial documentation needed by DHS; (4) provide information regarding freedom of choice of nursing facility versus CHOICES HCBS, both verbally and in writing, and obtain a Freedom of Choice form signed and dated by the member or his/her representative; (5) provide detailed information and signed acknowledgement of understanding regarding a CHOICES member’s responsibility with respect to payment of patient liability amounts, including, as applicable, the potential consequences for non-payment of patient liability which may include loss of the member’s current nursing facility or CBRA provider or MCO, disenrollment from CHOICES, and to the extent the member’s eligibility is dependent on receipt of long-term care services, possible loss of eligibility for TennCare; and (6) for members who want to receive nursing facility services, provide information regarding the completion of all PASRR requirements prior to nursing facility admission and conduct the level I PASRR screening; (7) for members who are seeking CHOICES HCBS, the care coordinator, shall: (a) conduct a risk assessment using a tool and protocol specified by TENNCARE and shall develop, as applicable, a risk agreement that shall be signed and dated by the member or his/her representative and which shall include identified risks to the member, the consequences of such risks, strategies to mitigate the identified risks, and the member’s decision regarding his/her acceptance of risk; (b) make a determination regarding whether the person’s needs can be safely and effectively met in the community and at a cost that does not exceed nursing facility care, and provide explanation to the member regarding the individual cost neutrality cap, including that a change in needs or circumstances that would result in the cost neutrality cap being exceeded or that would result in the CONTRACTOR’s inability to safely and effectively meet the member’s needs in the community and within the cost neutrality cap may result in the member’s disenrollment from CHOICES Group 2, in which case, the member’s care coordinator will assist with transition to a more appropriate care delivery setting; and (c) provide information regarding consumer direction and obtain written confirmation of the member’s decision regarding participation in consumer direction; and (8) for all members, provide information regarding choice of contract providers, subject to the provider’s availability and willingness to timely deliver services, and obtain signed documentation of the member’s choice of contract providers. |
| 2.9.6.3.10 | If the member does not meet appear to meet CHOICES enrollment criteria, the care coordinator may advise the member verbally: (1) that he/she does not appear to meet the criteria for enrollment in CHOICES; but shall also advise the member (2) that he/she has the right to continue with the CHOICES intake process and, if determined not eligible, to receive notice of such denial, including the member’s due process right to a fair hearing. |
| 2.9.6.3.10.1 | The decision to discontinue the CHOICES intake process must be made by the member or the member’s representative and the CONTRACTOR shall not encourage the member or member’s representative to discontinue the process; |
| 2.9.6.3.10.2 | Upon the member’s decision to continue the CHOICES intake, the care coordinator shall continue the intake process and complete all required activities, including submission of the level of care to TENNCARE; or |
| 2.9.6.3.10.3 | Upon the member’s decision to discontinue the CHOICES intake process, the care coordinator shall, in the manner prescribed by TENNCARE, document the member’s decision to terminate the CHOICES intake process, including the member’s or representative’s signature and date. The CONTRACTOR shall maintain this documentation in the member’s record and provide a copy to the member/representative. |
| 2.9.6.3.10.4 | The CONTRACTOR shall provide the member with information about how to initiate a new CHOICES screening and intake process in the future. |
| 2.9.6.3.11 | If, during the face-to-face intake visit the member or the member’s representative elects to terminate the intake process for any other reason (e.g., estate recovery, patient liability, or does not need the services available through CHOICES), the care coordinator shall, in the manner prescribed by TENNCARE, document the member’s decision to terminate the CHOICES intake process, including the member’s or representative’s signature and date. The CONTRACTOR shall maintain this documentation in the member’s record and provide a copy to the member/representative. |
| 2.9.6.3.11.1 | The decision to discontinue the CHOICES intake process must be made by the member or the member’s representative and the CONTRACTOR shall not encourage the member or member’s representative to discontinue the process; |
| 2.9.6.3.11.2 | The CONTRACTOR shall provide the member with information about how to initiate a new CHOICES screening and intake process in the future. |
| 2.9.6.3.12 | For CHOICES referrals by or on behalf of a potential CHOICES member, regardless of referral source, the care coordinator shall conduct the face-to-face intake visit and shall develop a plan of care, as appropriate (see Section 2.9.6.6), within ten (10) business days of receipt of such referral, unless a later date is requested by the member, which shall be documented in writing in the CHOICES intake record. |
| 2.9.6.3.13 | For members identified by the CONTRACTOR as potentially eligible for CHOICES by means other than referral, the care coordinator shall conduct the face-to-face intake visit and shall develop a plan of care, as appropriate (see Section 2.9.6.6), within thirty (30) days of identification of the member as potentially eligible for CHOICES. For persons identified through notification of hospital admission, the CONTRACTOR shall coordinate with the hospital discharge planner to determine whether long-term care services may be needed upon discharge, and if so, complete all applicable screening and/or intake processes immediately to facilitate timely transition to the most integrated and cost effective long-term care delivery setting appropriate for the member’s needs. |
| 2.9.6.3.14 | Once completed, the CONTRACTOR shall submit the level of care and, for members requesting CHOICES HCBS, documentation, as specified by TENNCARE, to verify that the member’s needs can be safely and effectively met in the community and within the cost neutrality cap to TENNCARE as soon as possible but no later than five (5) business days of the face-to-face visit. The CONTRACTOR shall make every effort to obtain supporting documentation required for the level of care in a timely manner and shall document in writing the cause of any delay in the submission of the required documentation to TENNCARE, including the CONTRACTOR’s actions to mitigate such delay. The CONTRACTOR shall be responsible for ensuring that the level of care is accurate and complete, satisfies all technical requirements specified by TENNCARE, and accurately reflects the member’s current medical and functional status based on information gathered, at a minimum, from the member, his or her representative, the Care Coordinator’s direct observations, and the history and physical or other medical records which shall be submitted with the application. The CONTRACTOR shall note in the level of care any discrepancies between these sources of information, and shall provide explanation regarding how the CONTRACTOR addressed such discrepancies in the level of care. |
| 2.9.6.3.15 | If the member is seeking access to CHOICES HCBS through enrollment in CHOICES Group 2 and the enrollment target for CHOICES Group 2 has been reached, the CONTRACTOR shall notify TENNCARE, at the time of submission of the level of care and needs assessment and plan of care, as appropriate, whether the person shall be placed on a waiting list for CHOICES Group 2. If the CONTRACTOR wishes to enroll the person in CHOICES Group 2 as a cost effective alternative (CEA) to nursing facility care that would otherwise be provided, the CONTRACTOR shall submit to TENNCARE the following: |
| 2.9.6.3.15.1 | A written summary of the CONTRACTOR’s CEA determination, including an explanation of the member’s circumstances which warrant the immediate provision of nursing facility services unless CHOICES HCBS are immediately available. |
| 2.9.6.3.15.2 | TENNCARE may request additional information as needed to confirm the CONTRACTOR’s CEA determination and/or provider capacity to meet the member’s needs, and shall, only upon receipt of satisfactory documentation, enroll the member in CHOICES. |
| 2.9.6.3.16 | The CONTRACTOR shall be responsible for (1) advising members who appear to meet the nursing facility level of care that are seeking access to CHOICES HCBS through enrollment in CHOICES Group 2 when an enrollment target has been (or will soon be) reached; (2) advising such persons that they may choose to receive nursing facility services if CHOICES HCBS are not immediately available; (3) determining whether the person wants nursing facility services if CHOICES HCBS are not immediately available; and (4) at the CONTRACTOR’s sole discretion, making a determination regarding whether enrollment in Group 2 constitutes a CEA because the immediate provision of nursing facility services will otherwise be required and submitting appropriate documentation to TENNCARE if there is a waiting list for CHOICES Group 2 but the CONTRACTOR chooses to enroll a member in Group 2 as a CEA (see Section 2.9.6.3.13.1). |
| 2.9.6.3.17 | The State will be responsible for determining TennCare categorical and financial eligibility and level of care and enrolling eligible TennCare members into CHOICES. |
| 2.9.6.3.18 | TENNCARE will notify the CONTRACTOR via the outbound 834 enrollment file when a person has been enrolled in CHOICES and, if the member is enrolled in CHOICES, the member’s CHOICES Group and applicable patient liability amounts (see Section 2.6.7). For members in CHOICES Group 2, TENNCARE will notify the CONTRACTOR of the member’s cost neutrality cap (see definition in Section 1 and see Section 2.6.1.5.2.3), which shall be the average cost of Level 1 nursing facility care unless a higher cost neutrality cap is established by TENNCARE based on information submitted by the AAAD or MCO (as applicable) in the level of care. |
| 2.9.6.3.19 | For all newly enrolled CHOICES Group 1 members, the CONTRACTOR shall reimburse NF services in accordance with the level of nursing facility services or reimbursement approved by TENNCARE, and as of the effective date of CHOICES enrollment, except that the CONTRACTOR may reimburse a lesser level of service which such lesser level of service is billed by the facility. |
| 2.9.6.3.20 | For the CONTRACTOR’s current members enrolled into CHOICES Group 2, the member’s Care Coordinator shall within ten (10) business days of notice of the member’s enrollment in CHOICES Group 2, authorize and initiate CHOICES HCBS. |
| 2.9.6.3.20.1 | For purposes of the CHOICES program, service authorizations for CHOICES HCBS shall include the amount, frequency, and duration of each service to be provided, and the schedule at which such care is needed, as applicable; and other relevant information as prescribed by TENNCARE. The CONTRACTOR may decide whether it will issue service authorizations for nursing facility services, or whether it will instead process claims for such services in accordance with the level of care and/or reimbursement (including the duration of such level of care and/or reimbursement) approved by TENNCARE (see Section 2.14.1.12), except that the CONTRACTOR may reimburse a lesser level of service when such lesser level of service is billed by the facility. |
| 2.9.6.3.20.2 | The CONTRACTOR shall provide at least verbal notice to the member prior to initiation of CHOICES HCBS identified in the plan of care regarding any change in providers selected by the member for each CHOICES HCBS; including the reason such change has been made. If the CONTRACTOR is unable to place a member in the nursing facility or community-based residential alternative setting requested by the member, the care coordinator shall meet with the member and his/her representative to discuss the reasons why the member cannot be placed with the requested facility and the available options and identify an alternative facility. |
| 2.9.6.3.20.3 | If the CONTRACTOR is unable to initiate any long-term care service within the timeframes specified in this Agreement, the CONTRACTOR shall issue written notice to the member, documenting the service(s) that will be delayed, the reasons for the delay and the date the service(s) will start, and shall make good faith efforts to ensure that services are provided as soon as practical. |
| 2.9.6.3.20.4 | For members enrolled in CHOICES Groups 1 or 2 who are, upon CHOICES enrollment, receiving nursing facility or community-based residential alternative services from a contract provider, the CONTRACTOR shall authorize such services from the current provider as of the effective date of CHOICES enrollment. The CONTRACTOR shall not move members enrolled in CHOICES Groups 1 or 2 who are, upon CHOICES enrollment, receiving services in a nursing facility or community-based residential alternative setting to another facility unless: (1) the member or his/her representative specifically requests to move, which shall be documented in the member’s file; (2) the member or his/her representative provides written consent to move based on quality or other concerns raised by the CONTRACTOR, which shall not include the nursing facility’s rate of reimbursement; or (3) the facility where the member is residing is not a contract provider; if the community-based residential facility where the member is currently residing is not a contract provider, the CONTRACTOR shall provide continuation of services in such facility for at least thirty (30) days, which shall be extended as necessary to ensure continuity of care pending the facility’s contracting with the CONTRACTOR or the member’s transition to a contract facility; if the member is transitioned to a contract facility, the CONTRACTOR shall facilitate a seamless transition to the new facility; if the nursing facility where the member is currently residing is a non-contract provider, the CONTRACTOR shall (a) authorize continuation of the services pending enrollment of the facility as a contract provider (except a facility excluded for a 2-year period when the facility has withdrawn from Medicaid participation); (b) authorize continuation of the services pending facilitation of the member’s transition to a contract facility, subject to the member’s agreement with such transition; or (c) may continue to reimburse services from the non-contract nursing facility in accordance with TennCare rules and regulations. |
| 2.9.6.3.20.5 | For members receiving nursing facility services, the care coordinator shall participate as appropriate in the nursing facility’s care planning process (see Section 2.9.6.5.1) and may supplement the facility’s plan of care as necessary (see Section 2.9.6.6.1). |
| 2.9.6.3.20.6 | The CONTRACTOR shall not divert or transition members in CHOICES Group 1 to CHOICES HCBS unless the member chooses to receive CHOICES HCBS as an alternative to nursing facility and is enrolled in Group 2. |
| 2.9.6.3.20.7 | The CONTRACTOR shall not admit a member enrolled in CHOICES Group 2 to a nursing facility unless: (1) the member requires a short-term nursing facility care stay; (2) the member chooses to transition to a nursing facility and enroll in Group 1; or (3) the CONTRACTOR determines that it cannot safely and effectively meet the needs of the member and at a cost that is less than the member’s cost neutrality cap and the member agrees to transition to a nursing facility and enroll in Group 1. |
| 2.9.6.3.20.8 | The CONTRACTOR shall not admit a member enrolled in CHOICES Group 3 to a nursing facility unless: (1) the member meets nursing facility level of care and is expected to require nursing facility services for ninety (90) days or less; or (2) the member meets nursing facility level of care, is expected to require nursing facility services for more than ninety (90) days and chooses to transition to a nursing facility and enroll in Group 1. |
| 2.9.6.3.2 | 1 TENNCARE may establish, pursuant to policies and protocols for management of waiting lists, alternative timeframes for completion of specified intake functions and activities for persons when there is a waiting list. |
32. Section 2.9.6.4.4 shall be deleted and replaced as follows:
| 2.9.6.4.4 | The CONTRACTOR may utilize a care coordination team approach to performing care coordination activities prescribed in Section 2.9.6. For each CHOICES member, the CONTRACTOR’s care coordination team shall consist of the member’s care coordinator and specific other persons with relevant expertise and experience appropriate to address the needs of CHOICES members. Care coordination teams shall be discrete entities within the CONTRACTOR’s organizational structure dedicated to fulfilling CHOICES care coordination functions. The CONTRACTOR shall establish policies and procedures that specify, at a minimum: the composition of care coordination teams; the tasks that shall be performed directly by the care coordinator as specified in this Agreement, including needs assessment, development of the plan of care, and all minimum care coordination contacts; the tasks that may be performed by the care coordinator or the care coordination team; measures taken to ensure that the care coordinator remains the member’s primary point of contact for the CHOICES program and related issues; escalation procedures to elevate issues to the care coordinator in a timely manner; and measures taken to ensure that if a member needs to reach his/her care coordinator specifically, calls that require immediate attention by a care coordinator are handled by a care coordinator and calls that do not require immediate attention are returned by the member’s care coordinator the next business day. The CONTRACTOR may elect to utilize specialized intake coordinators or intake teams for initial needs assessment and care planning activities. All intake activities identified as responsibilities of the care coordinator shall be completed by an individual who meets all of the requirements to be a care coordinator. Should the CONTRACTOR elect to utilize specialized intake coordinators or intake teams, the CONTRACTOR shall develop policies and procedures which specify how the contractor will coordinate a seamless transfer of information from the intake coordinator or team to the member’s care coordinator. |
33. Section 2.9.6.6.1.1 shall be amended by deleting the phrase “/care coordination team”.
| 2.9.6.6.1.1 | For members in CHOICES Group 1, the member’s care coordinator may: (1) rely on the plan of care developed by the nursing facility for service delivery instead of developing a plan of care for the member; and (2) supplement the nursing facility plan of care as necessary with the development and implementation of targeted strategies to improve health, functional, or quality of life outcomes (e.g., related to disease management or pharmacy management) or to increase and/or maintain functional abilities. A copy of any supplements to the nursing facility plan of care, and updates to such supplements, shall be maintained by the CONTRACTOR in the member’s file. |
34. Section 2.9.6.6.2.4 shall be deleted and replaced as follows:
| 2.9.6.6.2.4 | The plan of care developed for CHOICES members in Groups 2 and 3 prior to initiation of CHOICES HCBS shall at a minimum include: (1) pertinent demographic information regarding the member including the name and contact information of any representative and a list of other persons authorized by the member to have access to health care (including long-term care) related information and to assist with assessment, planning, and/or implementation of health care (including long-term care) related services and supports; (2) care, including specific tasks and functions, that will be performed by family members and other caregivers; (3) home health, private duty nursing, and longterm care services the member will receive from other payor sources including the payor of such services; (4) home health and private duty nursing that will be authorized by the CONTRACTOR, except in the case of persons enrolled on the basis of Immediate Eligibility who shall have access to services beyond the limited package of CHOICES HCBS (see Section 2.6.1.5.3) only upon determination of categorical and financial eligibility for TennCare; (5) CHOICES HCBS that will be authorized by the CONTRACTOR, including the amount, frequency, duration, and scope (tasks and functions to be performed) of each service to be provided, and the schedule at which such care is needed, as applicable; members enrolled on the basis of Immediate Eligibility shall have access only to a limited package of CHOICES HCBS (see Section 2.6.1.5.3) pending determination of categorical and financial eligibility for TennCare CHOICES however all identified needed services shall be listed in the plan of care; (6) a detailed back-up plan for situations when regularly scheduled HCBS providers are unavailable or do not arrive as scheduled; the back-up plan may include paid and unpaid supports and shall include the names and telephone numbers of persons and agencies to contact and the services provided by listed contacts; the CONTRACTOR shall assess the adequacy of the back-up plan; and (7) for CHOICES Group 2 members, the projected TennCare monthly and annual cost of home health and private duty nursing identified in (4) above, and the projected monthly and annual cost of CHOICES HCBS specified in (5) above, and for CHOICES Group 3 members, the projected total cost of CHOICES HCBS specified in (5) above, excluding the cost of minor home modifications. |
| 35. | Section 2.9.6.6.2.5.11 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 36. | Section 2.9.6.6.2.6 shall be amended by adding a new sentence as follows: |
| 2.9.6.6.2.6 | The member’s care coordinator/care coordination team shall ensure that the member reviews, signs and dates the plan of care as well as any updates. The care coordinator shall also sign and date the plan of care, along with any updates. |
| 37. | Sections 2.9.6.6.2.8 and 2.9.6.6.2.9 shall be deleted and replaced as follows: |
| 2.9.6.6.2.8 | Within five (5) business days of completing a reassessment of a member’s needs, the member’s care coordinator shall update the member’s plan of care as appropriate, and the CONTRACTOR shall authorize and initiate CHOICES HCBS in the updated plan of care. The CONTRACTOR shall comply with requirements for service authorization in Section 2.9.6.2.5.10, change of provider in Section 2.9.6.2.5.11, and notice of service delay in Section 2.9.6.2.5.12. |
| 2.9.6.6.2.9 | The member’s care coordinator shall inform each member of his/her eligibility end date and educate members regarding the importance of maintaining TennCare CHOICES eligibility, that eligibility must be redetermined at least once a year, and that members receiving CHOICES HCBS will be contacted by TENNCARE or its designee near the date a redetermination is needed to assist them with the process, e.g., collecting appropriate documentation and completing the necessary forms. |
38. Section 2.9.6.7.2.1 shall be amended by deleting the phrase “in CHOICES Group 1”.
| 2.9.6.7.2.1 | Members who are waiting for placement in a nursing facility; |
39. Sections 2.9.6.8 through 2.9.6.8.22 shall be deleted and replaced as follows:
| 2.9.6.8 | Nursing Facility-to-Community Transition |
| 2.9.6.8.1 | The CONTRACTOR shall develop and implement methods for identifying members who may have the ability and/or desire to transition from a nursing facility to the community. Such methods shall include, at a minimum: |
| 2.9.6.8.1.1 | Referrals, including but not limited to, treating physician, nursing facility, other providers, community-based organizations, family, and self-referrals; |
| 2.9.6.8.1.2 | Identification through the care coordination process, including but not limited to: assessments, information gathered from nursing facility staff or participation in Grand Rounds (as defined in Section 1); and |
| 2.9.6.8.1.3 | Review and analysis of members identified by TENNCARE based on Minimum Data Set (MDS) data from nursing facilities. |
| 2.9.6.8.2 | For transition referrals by or on behalf of a nursing facility resident, regardless of referral source, the CONTRACTOR shall ensure that within fourteen (14) days of the referral a care coordinator conducts an in-facility visit with the member to determine the member’s interest in and potential ability to transition to the community, and provide orientation and information to the member regarding transition activities. The member’s care coordinator/care coordination team shall document in the member’s case file that transition was discussed with the member and indicate the member’s wishes as well as the member’s potential for transition. The CONTRACTOR shall not require a member to transition when the member expresses a desire to continue receiving nursing facility services. |
| 2.9.6.8.3 | For identification by the CONTRACTOR by means other than referral or the care coordination process of a member who may have the ability and/or desire to transition from a nursing facility to the community, the CONTRACTOR shall ensure that within ninety (90) days of such identification a care coordinator conducts an in-facility visit with the member to determine whether or not the member is interested in and potential ability to pursue transition to the community. The member’s care coordinator/care coordination team shall document in the member’s case file that transition was discussed with the member and indicate the member’s wishes as well as the member’s potential for transition. The CONTRACTOR shall not require a member to transition when the member expresses a desire to continue receiving nursing facility services. |
| 2.9.6.8.4 | If the member wishes to pursue transition to the community, within fourteen (14) days of the initial visit (see Sections 2.9.6.8.2 and 2.9.6.8.3 above) or within fourteen (14) days of identification through the care coordination process, the care coordinator shall conduct an in- facility assessment of the member’s ability and/or desire to transition using tools and protocols specified or prior approved in writing by TENNCARE. This assessment shall include the identification of any barriers to a safe transition. |
| 2.9.6.8.5 | As part of the transition assessment, the care coordinator shall conduct a risk assessment using a tool and protocol specified by TENNCARE, discuss with the member the risk involved in transitioning to the community and shall begin to develop, as applicable, a risk agreement that shall be signed and dated by the member or his/her representative and which shall include identified risks to the member, the consequences of such risks, strategies to mitigate the identified risks, and the member’s decision regarding his/her acceptance of risk as part of the plan of care. The risk agreement shall include the frequency and type of care coordinator contacts that exceed the minimum contacts required (see Section 2.9.6.9.4), to mitigate any additional risks associated with transition and shall address any special circumstances due to transition. The member’s care coordinator/care coordination team shall also make a determination regarding whether the member’s needs can be safely and effectively met in the community and at a cost that does not exceed nursing facility care. The member’s care coordinator shall explain to the member the individual cost neutrality cap and notification process and obtain a signed acknowledgement of understanding by the member or his/her representative that a change in a member’s needs or circumstances that would result in the cost neutrality cap being exceeded or that would result in the CONTRACTOR’s inability to safely and effectively meet a member’s needs in the community and within the cost neutrality cap may result in the member’s disenrollment from CHOICES Group 2, in which case, the CONTRACTOR will assist with transition to a more appropriate care delivery setting. |
| 2.9.6.8.6 | For those members whose transition assessment indicates that they are not candidates for transition to the community, the care coordinator shall notify them in accordance with the specified transition assessment protocol. |
| 2.9.6.8.7 | For those members whose transition assessment indicates that they are candidates for transition to the community, the care coordinator shall facilitate the development of and complete a transition plan within fourteen (14) days of the member’s transition assessment. |
| 2.9.6.8.8 | The care coordinator shall include other individuals such as the member’s family and/or caregiver in the transition planning process if the member requests and/or approves, and such persons are willing and able to participate. |
| 2.9.6.8.9 | As part of transition planning, prior to the member’s physical move to the community, the care coordinator shall visit the residence where the member will live to conduct an on-site evaluation of the physical residence and meet with the member’s family or other caregiver who will be residing with the member (as appropriate). The care coordinator shall include in the transition plan activities and/or services needed to mitigate any perceived risks in the residence including but not limited to an increase in face-to-face visits beyond the minimum required contacts in Sections 2.9.6.8.18 and 2.9.6.8.17. |
| 2.9.6.8.10 | The transition plan shall address all services necessary to safely transition the member to the community and include at a minimum member needs related to housing, transportation, availability of caregivers, and other transition needs and supports. The transition plan shall also identify any barriers to a safe transition and strategies to overcome those barriers. |
| 2.9.6.8.11 | The CONTRACTOR shall approve the transition plan and authorize any covered or cost effective alternative services included in the plan within ten (10) business days of completion of the plan. The transition plan shall be fully implemented within ninety (90) days from approval of the transition plan, except under extenuating circumstances which must be documented in writing. |
| 2.9.6.8.12 | The member’s care coordinator shall also complete a plan of care that meets all criteria described in Section 2.9.6.6 for members in CHOICES Groups 2 and 3 including but not limited to completing a comprehensive needs assessment, completing and signing the risk agreement and making a final determination of cost neutrality. The plan of care shall be authorized and initiated prior to the member’s transition to the community. |
| 2.9.6.8.13 | The CONTRACTOR shall not prohibit a member from transitioning to the community once the member has been counseled regarding risk. However, the CONTRACTOR may determine that the member’s needs cannot be safely and effectively met in the community and at a cost that does not exceed nursing facility care. In such case, the CONTRACTOR shall seek written review and approval from TENNCARE prior to denial of any member’s request to transition to the community. If TENNCARE approves the CONTRACTOR’s request, the CONTRACTOR shall notify the member in accordance with TennCare rules and regulations and the transition assessment protocol, and the member shall have the right to appeal the determination (see Section 2.19.3.12 of this Agreement). |
| 2.9.6.8.14 | Once completed, the CONTRACTOR shall submit to TENNCARE documentation, as specified by TENNCARE to verify that the member’s needs can be safely and effectively met in the community and within the cost neutrality cap. Before transitioning a member the CONTRACTOR shall verify that the member has been approved for enrollment in CHOICES Group 2 effective as of the planned transition date. |
| 2.9.6.8.15 | The member’s care coordinator/care coordination team shall monitor all aspects of the transition process and take immediate action to address any barriers that arise during transition. |
| 2.9.6.8.16 | For members transitioning to a setting other than a community-based residential alternative setting, the care coordinator/care coordination team shall upon transition utilize the EVV system to monitor the initiation and daily provision of services in accordance with the member’s new plan of care, and shall take immediate action to resolve any service gaps (see definition in Section 1). |
| 2.9.6.8.17 | For members who will live independently in the community or whose on-site visit during transition planning indicated an elevated risk, within the first twenty-four (24) hours, the care coordinator shall visit the member in his/her residence. During the initial ninety (90) day post-transition period, the care coordinator shall conduct monthly face-to-face in-home visits to ensure that the plan of care is being followed, that the plan of care continues to meet the member’s needs, and the member has successfully transitioned to the community. |
| 2.9.6.8.18 | For members transitioning to a community-based residential alternative setting or who will live with a relative or other caregiver, within the first twenty-four (24) hours the care coordinator shall contact the member and within seven (7) days after the member has transitioned to the community, the care coordinator shall visit the member in his/her new residence. During the initial ninety (90) day post-transition period, the care coordinator shall (1) at a minimum, contact the member by telephone each month to ensure that the plan of care is being followed, that the plan of care continues to meet the member’s needs, and the member has successfully transitioned to the community; and (2) conduct additional face-to-face visits as necessary to address issues and/or concerns and to ensure that the member’s needs are met. |
| 2.9.6.8.19 | The CONTRACTOR shall monitor hospitalizations and nursing facility re-admission for members who transition from a nursing facility to the community to identify issues and implement strategies to improve transition outcomes. |
| 2.9.6.8.20 | The CONTRACTOR shall be permitted to coordinate or subcontract with local community- based organizations to assist in the identification, planning and facilitation processes related to nursing facility-to-community transitions that are not specifically assigned to the care coordinator. |
| 2.9.6.8.21 | The CONTRACTOR shall develop and implement any necessary assessment tools, transition plan templates, protocols, or training necessary to ensure that issues that may hinder a member’s successful transition are identified and addressed. Any tool, template, or protocol must be prior approved in writing by TENNCARE. |
| 2.9.6.8.22 | To facilitate nursing facility to community transition, the CONTRACTOR may elect to use specialized transition coordinators or transition teams. All transition activities identified as responsibilities of the care coordinator shall be completed by an individual who meets all of the requirements to be a care coordinator. |
| 2.9.6.8.23 | The CONTRACTOR shall implement policies and processes necessary to ensure that it is aware when a member is admitted to or discharged from a NF in order to facilitate care planning and as seamless a transition as possible, and to ensure timely notification to TENNCARE and other entities (e.g., DHS) as appropriate. |
| 2.9.6.8.23.1 | The CONTRACTOR shall require NFs to notify the CONTRACTOR of all NF discharges, transfers between NFs, or elections of hospice services in a NF. |
| 2.9.6.8.23.2 | The CONTRACTOR shall, in a manner prescribed by TENNCARE notify: a) TENNCARE of all NF discharges and elections of hospice services in a NF; b) DHS of all NF discharges and transfers between NFs; and c) receiving NFs of all applicable level of care information when a member is transferring between NFs. |
| 2.9.6.8.23.3 | The CONTRACTOR shall conduct a census at least semi-annually at no less than 120- day intervals or as frequently as necessary to confirm the residency status and Group assignment of all CHOICES members (i.e., Group 1 receiving services in a NF or Group 2 receiving HCBS or short-term NF services). The CONTRACTOR shall take actions as necessary to address any discrepancies when a CHOICES member is found to no longer be receiving LTC services, or is receiving services in a different service delivery setting, e.g., NF, HCBS, or hospice in a NF, including, as appropriate, disenrollment from CHOICES and/or enrollment in a different CHOICES Group. |
| 2.9.6.8.23.4 | The CONTRACTOR shall monitor all short-term NF stays for Group 2 members and shall ensure that the member is transitioned from Group 2 to Group 1 at any time a) it is determined that the stay will not be short-term and the member will not transition back to the community; and b) prior to exhausting the 90-day short-term NF benefit covered for CHOICES Group 2 members. |
| 40. | Section 2.9.6.9.1.1 shall be amended by adding a new Section 2.9.6.9.1.1.5 as follows and renumbering the existing Section 2.9.6.9.1.1 accordingly, including any references thereto. |
| 2.9.6.9.1.1.5 | In the manner prescribed by TENNCARE, facilitate transfers between nursing facilities which, at a minimum, includes notification to the receiving facility of the member’s level of care, and notification to DHS; and |
| 41. | The newly renumbered Section 2.9.6.9.1.1.6 shall be amended by adding a new Section 2.9.6.9.1.1.6.5 as follows and renumbering the existing Section 2.9.6.9.1.1.6 accordingly, including any references thereto. |
| 2.9.6.9.1.1.6.5 | Frequent emergency department utilization; or |
| 42. | Section 2.9.6.9.2.1.2 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 43. | Section 2.9.6.9.2.1.5 shall be deleted and replaced as follows: |
| 2.9.6.9.2.1.5 | For members in CHOICES Group 2, each time a member’s plan of care is updated to change the level or type of service, document in accordance with TENNCARE policy that the projected total cost of CHOICES HCBS, home health care and private duty nursing is less than the member’s cost neutrality cap. If a member’s medical condition has changed such that a different cost neutrality cap may be appropriate, the CONTRACTOR shall, in the manner prescribed by TENNCARE, submit to TENNCARE a request to update the member’s cost neutrality cap, including documentation specified by TENNCARE to support such request. The CONTRACTOR shall monitor utilization to identify members who may exceed the cost neutrality cap and to intervene as necessary to maintain the member’s community placement. The CONTRACTOR shall also educate members in CHOICES Group 2 about the cost neutrality cap and what will happen if the cap is met; |
| 44. | Sections 2.9.6.9.2.1.6 and 2.9.6.9.2.1.7 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 45. | Section 2.9.6.9.2.1.15 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 46. | Sections 2.9.6.9.3.1.1 and 2.9.6.9.3.1.1.1 shall be deleted and replaced as follows: |
| 2.9.6.9.3.1.1 | In the manner prescribed by TENNCARE, conduct a level of care reassessment at least annually and within five (5) business days of the CONTRACTOR’s becoming aware that the member’s functional or medical status has changed in a way that may affect level of care eligibility. |
| 2.9.6.9.3.1.1.1 | If the level of care assessment indicates a change in the level of care or if the assessment was prompted by a request by a member, a member’s representative or caregiver or another entity for a change in level of services, the level of care shall be forwarded to TENNCARE for determination; |
47. Section 2.9.6.9.4.3.2 through 2.9.6.9.4.3.8 shall be deleted and replaced as follows:
| 2.9.6.9.4.3.2 | Members who are newly admitted to a nursing facility when the admission has not been authorized or arranged by the CONTRACTOR, shall receive a face-to-face visit from their care coordinator within ten (10) days of notification of admission. |
| 2.9.6.9.4.3.3 | Members in CHOICES Group 2 who have transitioned from a nursing facility to the community shall be contacted per the applicable timeframe specified in Section 2.9.6.8. |
| 2.9.6.9.4.3.4 | Within five (5) business days of scheduled initiation of services, the member’s care coordinator/care coordination team shall contact members in CHOICES Groups 2 and 3 who begin receiving CHOICES HCBS after the date of enrollment in CHOICES to confirm that services are being provided and that the member’s needs are being met (such initial contact may be conducted by phone). |
| 2.9.6.9.4.3.5 | Within five (5) business days of scheduled initiation of CHOICES HCBS in the updated plan of care, the member’s care coordinator/care coordination team shall contact members in CHOICES Groups 2 and 3 to confirm that services are being provided and that the member’s needs are being met (such initial contact may be conducted by phone). |
| 2.9.6.9.4.3.6 | Members in CHOICES Group 1 (who are residents of a nursing facility) shall receive a face-to-face visit from their care coordinator at least twice a year with an interval of at least one-hundred and twenty (120) days between visits. |
| 2.9.6.9.4.3.7 | Members in CHOICES Group 2 shall be contacted by their care coordinator at least monthly either in person or by telephone with an interval of at least fourteen (14) days between contacts. These members shall be visited in their residence face-to-face by their care coordinator at least quarterly with an interval of at least sixty (60) days between visits. |
| 2.9.6.9.4.3.8 | Members in CHOICES Group 3 shall be contacted by their care coordinator at least quarterly either in person or by telephone with an interval of at least sixty (60) days between contacts. These members shall be visited in their residence face-to-face by their care coordinator a minimum of two (2) times per year with an interval of at least one- hundred (120) days between visits. |
48. Section 2.9.6.9.6.3.3 through 2.9.6.9.6.3.7 shall be deleted and replaced as follows:
| 2.9.6.9.6.3.3 | Written confirmation of the member’s decision regarding participation in consumer direction of eligible CHOICES HCBS; |
| 2.9.6.9.6.3.4 | For members in CHOICES Group 2, a completed risk assessment and a risk agreement signed and dated by the member or his/her representative; |
| 2.9.6.9.6.3.5 | For members in CHOICES Group 2, the cost neutrality cap provided by TENNCARE, and a determination by the CONTRACTOR that the projected cost of CHOICES HCBS, home health, and private duty nursing services will not exceed the member’s cost neutrality cap; and |
49. Section 2.9.6.9.6.4.1 through 2.9.6.9.6.4.3 shall be deleted and replaced as follows:
| 2.9.6.9.6.4.1 | For CHOICES members age 21 and older in Groups 1 and 2, a Freedom of Choice form signed and dated by the member or his/her representative; |
| 2.9.6.9.6.4.2 | Evidence that a care coordinator provided the member with CHOICES member education materials (see Section 2.17.7 of this Agreement), reviewed the materials, and provided assistance with any questions; |
| 2.9.6.9.6.4.3 | Evidence that a care coordinator provided the member with education about the member’s ability to use an advance directive and documentation of the member’s decision; |
50. Section 2.9.6.10 through 2.9.6.10.14 shall be deleted and replaced as follows:
| 2.9.6.10 | Additional Requirements for Care Coordination Regarding Consumer Direction of eligible CHOICES HCBS |
| 2.9.6.10.1 | In addition to the roles and responsibilities otherwise specified in this Section 2.9.6, the CONTRACTOR shall ensure that the following additional care coordination functions related to consumer direction of eligible CHOICES HCBS are fulfilled. |
| 2.9.6.10.2 | The CONTRACTOR shall be responsible for providing all needed eligible CHOICES HCBS using contract providers until all necessary requirements have been fulfilled in order to implement consumer direction of eligible CHOICES HCBS, including but not limited to: the FEA verifies that workers for these services meet all necessary requirements (see Section 2.9.7.6.1 of this Agreement); service agreements are completed and signed; and authorizations for consumer directed services are in place. The CONTRACTOR, in conjunction with the FEA, shall facilitate a seamless transition between contract providers and workers and ensure that there are no interruptions or gaps in services. |
| 2.9.6.10.3 | If a member elects not to receive eligible CHOICES HCBS using contract providers until all necessary requirements have been fulfilled in order to implement consumer direction of eligible CHOICES HCBS, the CONTRACTOR shall document this decision, including date and member/member’s representative’s signature, in the manner specified by TENNCARE. |
| 2.9.6.10.4 | If a member is interested in participating in consumer direction of eligible CHOICES HCBS and the member does not intend to appoint a representative, the care coordinator shall determine the extent to which the member may require assistance to direct his/her services (see Section 2.9.7.4.5). If the care coordinator determines that the member requires assistance to direct his/her services, based upon the results of a completed self-assessment instrument developed by TENNCARE, the care coordinator shall inform the member that he/she will need to designate a representative to assume the consumer direction functions on his/her behalf (see Section 2.9.7.4.5.1). |
| 2.9.6.10.5 | The member’s care coordinator/care coordination team shall ensure that the person identified to serve as the representative meets all qualifications (see Section 2.9.7.2.1) and that a representative agreement is completed and signed by the member prior to forwarding a referral to the FEA (see Section 2.9.7.4.7). |
| 2.9.6.10.6 | For members electing to participate in consumer direction, forward to the FEA a referral initiating the member’s participation in consumer direction of eligible CHOICES HCBS: (1) within two (2) business days of signing the representative agreement; or (2) if a representative is not designated by the member, within two (2) business days of completion of the self-assessment instrument and the care coordinator determines that the member does not require a representative to assist the member in directing his/her care. |
| 2.9.6.10.7 | For members electing to participate in consumer direction, the member’s care coordinator shall integrate the member’s back-up plan for consumer-directed workers (including any updates thereto) into the member’s back-up plan for services provided by contract providers, as applicable, and the member’s plan of care. The care coordinator shall review the back-up plan developed by the member or his/her representative (as applicable) for consumer direction to determine its adequacy to address the member’s needs, and shall monitor for late and missed visits and to ensure that the back-up plan was implemented timely and that the member’s needs are being met. |
| 2.9.6.10.8 | For members electing to participate in consumer direction, the member’s care coordinator shall reassess the adequacy of the member’s back-up plan for consumer direction on at least an annual basis which shall include any time there are changes in the type, amount, duration, scope of eligible CHOICES HCBS or the schedule at which such services are needed, changes in consumer- directed workers (when such workers also serve as a back-up to other workers) or changes in the availability of paid or unpaid back-up workers to deliver needed care |
| 2.9.6.10.9 | For members electing to participate in consumer direction, the member’s care coordinator shall develop and/or update, as applicable, a risk agreement which takes into account the member’s decision to participate in consumer direction, and which identifies any additional risks associated with the member’s decision to direct his/her services, the potential consequences of such risk, as well as measures to mitigate these risks. The member’s representative (if applicable) shall participate in the risk assessment process. The new or updated risk agreement, as applicable, shall be signed by the member (or the member’s representative, as applicable). The CONTRACTOR shall provide a copy of the risk agreement to the member/representative and the FEA. |
| 2.9.6.10.10 | On an ongoing basis, the CONTRACTOR shall ensure that needs reassessments and updates to the plan of care occur per requirements specified in Sections 2.9.6.9 of this Agreement. The care coordinator shall ensure that, for members participating in consumer direction, the member’s supports broker is invited to participate in these meetings. |
| 2.9.6.10.11 | Within two (2) business days of receipt of the notification from the FEA indicating that all requirements have been fulfilled and the date that the consumer direction can begin for a member, the CONTRACTOR shall forward to the FEA an authorization for consumer directed services for that member. Each authorization for consumer directed services shall include authorized service, authorized units of service, including amount, frequency and duration and the schedule at which services are needed, start and end dates, and service code(s). |
| 2.9.6.10.12 | The member’s care coordinator/care coordination team shall work with and coordinate with a member’s supports broker in implementing and monitoring consumer direction of eligible CHOICES HCBS (see Section 2.9.7.3.4). |
| 2.9.6.10.13 | The CONTRACTOR shall establish a process that allows for the efficient exchange of all relevant member information between the CONTRACTOR and the FEA. |
| 2.9.6.10.14 | The care coordinator shall determine a member’s interest in enrolling in or continuing to participate in consumer direction annually and shall document the member’s decision in the member’s plan of care. |
| 2.9.6.10.15 | If at anytime abuse or neglect is suspected, the member’s care coordinator or the FEA shall report the allegations to the CONTRACTOR within 24 hours in accordance with the CONTRACTOR’s abuse and neglect plan protocols. The notification shall include at a minimum: the member name; date of allegation reported and/or identified; description of issue; measures taken to mitigate risk; status of reporting to CPS or APS, as appropriate. If the allegation is in reference to a worker or representative, the FEA shall contact the member/representative to immediately release the worker or representative from his/her duties until the investigation is complete. The FEA shall notify the CONTRACTOR regarding this communication with the member/representative and the member or representative’s decision. The care coordinator shall work with the member to find a new representative and the FEA shall work with the member to find a suitable replacement worker, if applicable. If the allegations are substantiated as a result of the investigation, the representative or worker shall no longer be allowed to participate in the CHOICES program as a representative or worker. If the investigation is inconclusive, the member may elect to retain the worker or representative. The member’s care coordinator, with appropriate assistance from the FEA, shall make any updates to the member’s plan of care and/or risk assessment/risk agreement deemed necessary to help ensure the member’s health and safety, and the CONTRACTOR may initiate action to involuntary disenroll the member from consumer direction at any time the CONTRACTOR feels that the member’s decisions or actions constitute unreasonable risk such that the member’s needs can no longer be safely and effectively met in the community while participating in consumer direction. |
51. Section 2.9.6.11.5 shall be deleted and replaced as follows:
| 2.9.6.11.5 | While care coordination staffing ratios are not specified, the CONTRACTOR shall notify TENNCARE in writing of substantive changes to its Care Coordination Staffing Plan, including a variance of twenty (20) percent or more from the planned staffing ratio. TENNCARE may request changes in the CONTRACTOR’s Care Coordination Staffing Plan at any time it determines that the CONTRACTOR does not have sufficient care coordination staff to properly and timely perform its obligations under this Agreement. |
52. Sections 2.9.6.11.12 through 2.9.6.11.12.27 shall be deleted and replaced as follows:
| 2.9.6.11.12 | The CONTRACTOR shall provide initial training to newly hired care coordinators and ongoing training at least annually to care coordinators. Initial training topics shall include at a minimum: |
| 2.9.6.11.12.1 | The CHOICES program including a description of the CHOICES groups; eligibility for CHOICES enrollment; enrollment in CHOICES; enrollment targets for Groups 2 and 3, including reserve capacity and administration of waiting lists; and CHOICES benefits, including benefit limits, the individual cost neutrality cap for Group 2, the expenditure cap for Group 3, and the limited benefit package for members enrolled on the basis of Immediate Eligibility; |
| 2.9.6.11.12.2 | Facilitating CHOICES enrollment for current members; |
| 2.9.6.11.12.3 | Level of care and needs assessment and reassessment, development of a person-centered plan of care, and updating the plan of care including training on the tools and protocols; |
| 2.9.6.11.12.4 | Development and implementation of back-up plans; |
| 2.9.6.11.12.5 | Risk assessment and development of a member-specific risk agreement; 2.9.6.11.12.6 Consumer direction of eligible CHOICES HCBS; |
| 2.9.6.11.12.7 | Self-direction of health care tasks; |
| 2.9.6.11.12.8 | Coordination of care for duals; |
| 2.9.6.11.12.9 | Electronic visit verification; |
| 2.9.6.11.12.10 | Conducting a home visit and use of the monitoring checklist; |
| 2.9.6.11.12.11 | How to immediately identify and address service gaps; |
| 2.9.6.11.12.12 | Management of critical transitions (including hospital discharge planning); 2.9.6.11.12.13 Nursing facility diversion; |
| 2.9.6.11.12.14 | Nursing facility to community transitions, including training on tools and protocols; |
| 2.9.6.11.12.15 | Management of transfers between nursing facilities and CBRA facilities, including adult care homes; |
| 2.9.6.11.12.16 | Facilitation of transitions between CHOICES Groups; |
| 2.9.6.11.12.17 | For members in CHOICES Groups 1 and 2, as applicable, members’ responsibility regarding patient liability, including the consequences of not paying patient liability; |
| 2.9.6.11.12.18 | Alzheimer’s, dementia and cognitive impairments; 2.9.6.11.12.19 Traumatic brain injury; |
| 2.9.6.11.12.20 | Physical disabilities; |
| 2.9.6.11.12.21 | Disease management; |
| 2.9.6.11.12.22 | Behavioral health; |
| 2.9.6.11.12.23 | Evaluation and management of risk; |
| 2.9.6.11.12.24 | Identifying and reporting abuse/neglect (see Section 2.24.4); |
| 2.9.6.11.12.25 | Critical incident reporting (see Section 2.15.7); 2.9.6.11.12.26 Fraud and abuse, including reporting fraud and abuse; 2.9.6.11.12.27 Advance directives and end of life care; |
| 2.9.6.11.12.28 | HIPAA/HITECH; |
| 2.9.6.11.12.29 | Cultural competency; |
| 2.9.6.11.12.30 | Disaster planning; and |
| 2.9.6.11.12.31 | Available community resources for non-covered services. |
| 53. | Section 2.9.6.12.1.2 shall be amended by adding the words “level of care” in front of the word “reassessments” as follows: |
| 2.9.6.12.1.2 | Level of care assessments and level of care reassessments occur on schedule and are submitted to TENNCARE in accordance with requirements in Section 2.9.6.9.3.1.1; |
| 54. | Section 2.9.6.12.3 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 55. | Section 2.9.6.12 shall be amended by adding a new Section 2.9.6.12.4 and renumbering the existing Sections accordingly, including any references thereto. |
| 2.9.6.12.4 | The CONTRACTOR shall require, and shall conduct readiness review activities as necessary to confirm that the EVV system vendor has a plan in place and will be compliant with all ICD- 10 requirements in a timely manner; |
| 56. | Section 2.9.7 through 2.9.7.1.3.10 shall be deleted and replaced as follows: |
2.9.7 Consumer Direction of Eligible CHOICES HCBS
| 2.9.7.1 | General |
| 2.9.7.1.1 | The CONTRACTOR shall offer consumer direction of eligible CHOICES HCBS to all CHOICES Group 2 and 3 members who are determined by a care coordinator, through the needs assessment/reassessment process, to need attendant care, personal care, homemaker, in- home respite, companion care services and/or any other service specified in TennCare rules and regulations as available for consumer direction. (Companion care is only available for persons electing consumer direction of eligible CHOICES HCBS.) A service that is not specified in TennCare rules and regulations as available for consumer direction or that is not a CHOICES HCBS shall not be consumer directed. Consumer direction in CHOICES affords members the opportunity to have choice and control over how eligible CHOICES HCBS are provided, who provides the services and how much workers are paid for providing care, up to a specified maximum amount established by TENNCARE (see Section 2.9.7.6.11). Member participation in consumer direction of eligible CHOICES HCBS is voluntary. Members may elect to participate in or withdraw from consumer direction of eligible CHOICES HCBS at any time, service by service, without affecting their enrollment in CHOICES. To the extent possible, the member shall provide his/her care coordinator ten (10) days advance notice regarding his/her intent to no longer direct one or more eligible CHOICES HCBS or to withdraw from participation in consumer direction of eligible CHOICES HCBS entirely. The CONTRACTOR shall respond to the member’s request in keeping with the timeframes and processes set forth in this Section, in order to facilitate a seamless transition to appropriate service delivery. TENNCARE may establish reasonable limitations on the frequency with which members may opt into and out of consumer direction of eligible CHOICES HCBS. |
| 2.9.7.1.2 | Consumer direction is a process by which eligible CHOICES HCBS are delivered; it is not a service. If a member chooses not to direct his/her care, he/she shall receive authorized CHOICES HCBS through contract providers. While the denial of a member’s request to participate in consumer direction or the termination of a member’s participation in consumer direction gives rise to due process including the right to fair hearing, such appeals shall be processed by the TennCare Division of Long Term Care rather than the TennCare Solutions Units, which manages medical appeals pertaining to TennCare benefits (i.e., services). |
| 2.9.7.1.3 | Members who participate in consumer direction of eligible CHOICES HCBS choose either to serve as the employer of record of their workers or to designate a representative (see definition below in Section 2.9.7.2.1) to serve as the employer of record on his/her behalf. As the employer of record the member or his/her representative is responsible for the following: |
| 2.9.7.1.3.1 2.9.7.1.3.2 2.9.7.1.3.3 2.9.7.1.3.4 |
Recruiting, hiring and firing workers; Determining workers’ duties and developing job descriptions; Scheduling workers; Supervising workers; |
| 2.9.7.1.3.5 | Evaluating worker performance and addressing any identified deficiencies or concerns; |
| 2.9.7.1.3.6 | Setting wages from a range of rates established by TENNCARE; |
| 2.9.7.1.3.7 | Training workers to provide personalized care based on the member’s needs and preferences; |
| 2.9.7.1.3.8 | Ensuring that workers deliver only those services authorized, and reviewing and approving hours worked by consumer-directed workers; |
| 2.9.7.1.3.9 | Reviewing and ensuring proper documentation for services provided; and |
| 2.9.7.1.3.10 | Developing and implementing as needed a back-up plan to address instances when a scheduled worker is not available or fails to show up as scheduled. |
| 57. | Sections 2.9.7.2.2 and 2.9.7.2.4 shall be amended by adding the words “eligible CHOICES in front of the word “HCBS”. |
| 58. | Sections 2.9.7.3.2, 2.9.7.3.2.1, 2.9.7.3.3, and 2.9.7.3.11.6 shall be amended by adding the words “eligible CHOICES in front of the word “HCBS”. |
| 59. | Section 2.9.7.4 through 2.9.7.4.10.13 shall be deleted and replaced as follows: |
| 2.9.7.4 | Needs Assessment/Plan of Care Process |
| 2.9.7.4.1 | A CHOICES member may choose to direct needed eligible CHOICES HCBS at anytime: during CHOICES intake, through the needs assessment/reassessment and plan of care and plan of care update processes; and outside of these processes. The care coordinator shall assess the member’s needs for eligible CHOICES HCBS per requirements in Sections 2.9.6.2.4, 2.9.6.3 and 2.9.6.5, as applicable. The care coordinator shall use the plan of care process (including updates) to identify the eligible services that the member will direct and to facilitate the member’s enrollment in consumer direction of eligible CHOICES HCBS. |
| 2.9.7.4.2 | The CONTRACTOR shall obtain from the member a signed statement regarding the member’s decision to participate in consumer direction of eligible CHOICES HCBS. |
| 2.9.7.4.2.1 | The care coordinator shall assist the member in identifying which of the needed eligible CHOICES HCBS shall be consumer directed, provided by contract providers or a combination of both, in which case, there must be a set schedule which clearly defines when contract providers will be utilized. The CONTRACTOR shall not be expected or required to maintain contract providers “on standby” to serve in a back-up capacity for services a member has elected to receive through consumer direction. |
| 2.9.7.4.3 | If the member intends to direct one or more needed eligible CHOICES HCBS, throughout the period of time that consumer direction is being initiated, the CONTRACTOR shall arrange for the provision of needed CHOICES HCBS through contract providers in accordance with 2.9.6. The care coordinator shall obtain from the member his/her choice of contract providers who will provide CHOICES HCBS until such time as workers are secured and ready to begin delivering care through consumer direction. |
| 2.9.7.4.3.1 | If a member has been assessed to need companion care services, the CONTRACTOR shall identify non-residential services that will offer interim support to address the member’s needs and assist the member in obtaining contract providers for these services. |
| 2.9.7.4.4 | The CONTRACTOR shall be responsible for providing all needed eligible CHOICES HCBS using contract providers, including a back-up plan for such services, until all necessary requirements have been fulfilled in order to implement consumer direction of eligible CHOICES HCBS, including but not limited to: the FEA verifies that workers for these services meet all necessary requirements (see Section 2.9.7.6.1 of this Agreement); service agreements are completed and signed; and authorizations for consumer directed services are in place. The CONTRACTOR, in conjunction with the FEA, shall facilitate a seamless transition between contract providers and workers and ensure that there are no interruptions or gaps in services. |
| 2.9.7.4.5 | The care coordinator shall determine if the member will appoint a representative to assume the consumer direction functions on his/her behalf. If the member does not intend to appoint a representative, the care coordinator shall determine the extent to which a member requires assistance to participate in consumer direction of eligible CHOICES HCBS, based upon the results of the member’s responses to the self-assessment instrument developed by TENNCARE. The self-assessment instrument shall be completed by the member with assistance from the member’s care coordinator as appropriate. The care coordinator shall file the completed self-assessment in the member’s file. |
| 2.9.7.4.5.1 | If, based on the results of the self-assessment the care coordinator determines that a member requires assistance to direct his/her services, the care coordinator shall inform the member that he/she will need to designate a representative to assume the consumer direction functions on his/her behalf. |
| 2.9.7.4.5.2 | The CONTRACTOR shall forward to TENNCARE for disposition, pursuant to TennCare policy, any cases in which the CONTRACTOR plans to deny participation in consumer direction because a care coordinator has determined that the health, safety and welfare of the member would be in jeopardy if the member participates in consumer direction without a representative but the member does not want to appoint a representative to assist in directing his/her services. The CONTRACTOR shall abide by TENNCARE’s decision. |
| 2.9.7.4.6 | The member’s care coordinator/care coordination team shall ensure that the person identified to serve as the representative meets all qualifications (see Section 2.9.7.2.1 of this Agreement) and that a representative agreement is completed and signed by the member and the person prior to forwarding a referral to the FEA (see Section 2.9.7.4.7 below). |
| 2.9.7.4.7 | Within two (2) business days of signing the representative agreement or completion of the self-assessment instrument if the member has not designated a representative and the care coordinator determines that the member does not require a representative to assist the member in directing his/her care, the CONTRACTOR shall forward to the FEA a referral initiating the member’s participation in consumer direction of eligible CHOICES HCBS. The referral shall include at a minimum: the date of the referral; the member’s name, address, telephone number, and social security number (SSN); the name of the representative and telephone number (if applicable); member’s MCO ID number; member’s CHOICES enrollment date; eligible selected HCBS, including amount, frequency and duration of each by type; and care coordinator’s name and contact information. The CONTRACTOR shall also forward to the FEA a copy of the written confirmation of the member’s decision to participate in consumer direction of eligible CHOICES HCBS. Referrals shall be submitted electronically on a daily basis using the agreed upon data interface (either a standard electronic file transfer or the FEA’s web portal technology or both) and process. Referrals shall be submitted on a member-by-member basis. |
| 2.9.7.4.8 | Within two (2) business days of receipt of the referral, the FEA shall assign a supports broker to the member, notify the care coordinator of the assignment and provide the name and contact information of the supports broker. |
| 2.9.7.4.9 | Within five (5) days of receipt of the referral, the FEA shall contact the member to inform the member of his/her assigned supports broker, provide contact information for the supports broker, and to begin the process of initiating consumer direction of eligible CHOICES HCBS. |
| 2.9.7.4.10 | Back-up Plan for Consumer Direction and Updated Risk Assessment/Risk Agreement |
| 2.9.7.4.10.1 | The FEA shall assist the member/representative as needed in developing a back-up plan for consumer direction that adequately identifies how the member/representative will address situations when a scheduled worker is not available or fails to show up as scheduled. The member/representative (as applicable) shall have primary responsibility for the development and implementation of the back-up plan for consumer directed services. |
| 2.9.7.4.10.2 | The member/representative (as applicable) may not elect, as part of the back-up plan, to go without services. |
| 2.9.7.4.10.3 | The back-up plan for consumer direction shall include the names and telephone numbers of contacts (workers, agency staff, organizations, supports) for alternate care, the order in which each shall be notified and the services to be provided by contacts. Back-up contacts may include paid and unpaid supports; however, it is the responsibility of the member electing consumer direction and/or his/her representative to secure paid (as well as unpaid) back-up contacts who are willing and available to serve in this capacity. The CONTRACTOR shall not be expected or required to maintain contract providers “on standby” to serve in a back-up capacity for services a member has elected to receive through consumer direction. |
| 2.9.7.4.10.4 | All persons and/or organizations noted in the back-up plan for consumer direction shall be contacted by the member/representative to determine their willingness and availability to serve as back-up contacts. The FEA shall confirm with these persons and/or organizations to confirm their willingness and availability to provide care when needed, document confirmation in the member’s file and forward a copy of the documentation to the CONTRACTOR. |
| 2.9.7.4.10.5 | The member’s care coordinator shall integrate the member’s back-up plan for consumer-directed workers (including any updates thereto) into the member’s back-up plan for services provided by contract providers, as applicable, and the member’s plan of care. The care coordinator shall review the back-up plan developed by the member or his/her representative (as applicable) for consumer direction to determine its adequacy to address the member’s needs, and shall monitor for late and missed visits and to ensure that the back-up plan was implemented timely and that the member’s needs are being met. |
| 2.9.7.4.10.6 | The FEA shall assist the member or his/her representative (as applicable) in implementing the back-up plan for consumer direction as needed, monitor to ensure that the back-up plan is implemented and effectively working to address the member’s needs, and notify the care coordinator immediately regarding any concerns with the back-up plan or the member’s care. |
| 2.9.7.4.10.7 | The FEA shall assist the member or his/her representative (as applicable) in reviewing and updating the back-up plan for consumer direction at least annually and as frequently as necessary, which shall include any time there are changes in the type, amount, duration, scope of eligible CHOICES HCBS or the schedule at which such services are needed, changes in workers (when such workers also serve as a back-up to other workers) and changes in the availability of paid or unpaid back-up workers to deliver needed care. As part of the annual review of the back-up plan, the member or his/her representative and the FEA shall confirm that each person specified in the back-up plan continues to be willing and available to serve as back-up workers to deliver needed care and to perform the tasks and functions needed by the member. Any updates to the back-up plan for consumer direction shall be provided to the member’s care coordinator. |
| 2.9.7.4.10.8 | The FEA and the CONTRACTOR shall each file a copy of the back-up plan for consumer direction in the member’s file. |
| 2.9.7.4.10.9 | The member’s care coordinator shall reassess the adequacy of the member’s back-up plan for consumer direction on at least an annual basis which shall include any time there are changes in the type, amount, duration, scope of eligible CHOICES HCBS or the schedule at which such services are needed, changes in consumer-directed workers (when such workers also serve as a back-up to other workers) or changes in the availability of paid or unpaid back-up workers to deliver needed care. |
| 2.9.7.4.10.10 | The CONTRACTOR shall develop and/or update, as applicable, a risk agreement which takes into account the member’s decision to participate in consumer direction, and which identifies any additional risks associated with the member’s decision to direct his/her services, the potential consequences of such risk, as well as measures to mitigate these risks. The member/representative shall participate in the process. The member’s representative (if applicable) shall participate in the risk assessment process. Once a referral has been made to the FEA for consumer direction, the member’s supports broker should be involved in risk assessment and risk planning activities whenever possible. The new or updated risk agreement, as applicable, shall be signed by the member or his/her representative (as applicable). The CONTRACTOR, member/representative and FEA shall receive a copy of the risk agreement. The CONTRACTOR and the FEA shall each file a copy of the risk agreement in the member’s file. |
| 2.9.7.4.10.11 | The FEA shall notify the member’s care coordinator immediately when there are changes in the member’s needs and/or circumstances which warrant a reassessment of needs and/or risk, or changes to the plan of care or risk agreement. |
| 2.9.7.4.10.12 | The FEA shall assist the CONTRACTOR in identifying and addressing in the risk assessment and plan of care processes any additional risk associated with the member participating in consumer direction. |
| 2.9.7.4.10.13 | On an ongoing basis, the CONTRACTOR shall ensure that needs reassessments and updates to the plan of care occur per requirements specified in Sections 2.9.6.9 of this Agreement. The care coordinator shall ensure that the member’s supports broker is invited to participate in these meetings. |
60. Section 2.9.7.5 through 2.9.7.5.10.1 shall be deleted and replaced as follows:
| 2.9.7.5 | Authorizations for Consumer Directed Services and Service Initiation |
| 2.9.7.5.1 | Consumer direction of eligible CHOICES HCBS shall not be initiated until all requirements are fulfilled including but not limited to the following: (1) the FEA verifies that the member’s employer and related documentation is in order; (2) the FEA verifies that workers meet all qualifications, including participation in required training; (3) there is a signed service agreement specific to each individual worker (see Section 2.9.7.6.6 of this Agreement); and (4) the CONTRACTOR issues to the FEA an authorization for consumer directed services (see 2.9.7.5.6 below) for each service. |
| 2.9.7.5.2 | The FEA shall work with the member to determine the appropriate level of assistance necessary to recruit, interview and hire workers and provide the assistance. |
| 2.9.7.5.3 | Once potential workers are identified, the FEA shall verify that a potential worker meets all applicable qualifications (see Section 2.9.7.6.1 of this Agreement). |
| 2.9.7.5.4 | The FEA shall ensure that a service agreement is signed between the member or member’s representative and his/her worker within five (5) business days following the FEA’s verification that a worker meets all qualifications. |
| 2.9.7.5.5 | The FEA shall periodically update the member’s care coordinator of the status of completing required functions necessary to initiate consumer direction, including obtaining completed paperwork from the member/representative and obtaining workers for each identified consumer directed service and any anticipated timeframes by which qualified workers shall be secured and consumer directed services may begin. |
| 2.9.7.5.6 | The provision of consumer directed services shall begin as soon as possible but no longer than sixty (60) days from the date of the CONTRACTOR’s referral to the FEA, except due to circumstances beyond the control of the FEA. Prior to beginning the provision of consumer directed services, the FEA shall notify the CONTRACTOR that all requirements have been fulfilled, including verification of all worker qualifications, criminal background checks, signed service agreements, and that the member is ready to begin consumer direction of eligible CHOICES HCBS. Within two (2) business days of receipt of the notification from the FEA, the CONTRACTOR shall forward to the FEA an authorization for consumer directed services. Each authorization for consumer directed services shall include authorized service; authorized units of service, including amount, frequency and duration and, as appropriate, the schedule at which services are needed; start and end dates; and service code(s). Authorized units of service in a service authorization should reflect the units of measure specified by TENNCARE for the benefit (e.g. visits, hours, days). The CONTRACTOR shall submit authorizations electronically on at least a daily basis using the agreed upon data interface (which may include a standard electronic file transfer, the FEA’s web portal technology, the EVV system, or any combination thereof). |
| 2.9.7.5.7 | If initiation of consumer directed services does not begin within sixty (60) days from the date of the CONTRACTOR’s referral to the FEA, the FEA shall contact the CONTRACTOR regarding the cause of the delay and provide appropriate documentation to demonstrate efforts to meet the timeframe. The CONTRACTOR shall determine the appropriate next steps, including but not limited to whether additional time is needed or if the member is still interested in participating in consumer direction of eligible CHOICES HCBS. |
| 2.9.7.5.8 | Upon the scheduled start date of consumer directed services, the member’s care coordinator/care coordination team shall begin monitoring to ensure that services have been initiated and continue to be provided as authorized. This shall include ongoing monitoring via electronic visit verification to ensure that services are provided in accordance with the member’s plan of care, including the amount, frequency, duration and scope of each service, in accordance with the member’s service schedule. Upon the identification of any gaps in care, the member’s care coordinator/care coordination team shall contact the FEA who shall assist the member or his/her representative as needed in implementing the member’s back-up plan for consumer direction. |
| 2.9.7.5.9 | Within five (5) business days of the scheduled start date of consumer directed services as specified in the authorization of consumer directed services, a member of the care coordinator team shall contact the member or his/her representative to confirm that services are being provided and that the member’s needs are being met. |
| 2.9.7.5.10 | On an ongoing basis, in addition to requirements specified above in 2.9.7.5.3 – 2.9.7.5.9 above: |
| 2.9.7.5.10.1 | The CONTRACTOR shall develop and forward to the FEA a new authorization for consumer directed services when the following occur: a change in the number of service units, or the frequency or duration of service delivery, or a change in the schedule at which services are needed; or a change in the services to be provided through consumer direction, including the provision of a new service through consumer direction or termination of a service through consumer direction. |
| 61. | Sections 2.9.7.7.1, 2.9.7.7.4.1, and 2.9.7.8.5 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 62. | Section 2.9.7.9 through 2.9.7.9.9 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS” and by adding the words “outbound 834” in front of the words “enrollment file”. |
| 63. | Section 2.9.7.9.10.2 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS. |
| 64. | Section 2.9.14.6 shall be deleted and replaced and Section 2.9.14.7 shall be deleted in its entirety and the remaining Section 2.9.14 shall be renumbered accordingly, including any references thereto. |
| 2.9.14.6 | Area Agencies on Aging and Disability (AAADs) regarding intake of members new to both TennCare and CHOICES, and assisting CHOICES members in Groups 2 and 3 with the TennCare eligibility redetermination process; |
| 65. | Section 2.11.1.4.1 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 66. | Section 2.11.1.8.2 shall be amended by deleting the phrase “, including services”. |
| 2.11.1.8.2 | The CONTRACTOR is not required to provide non-emergency transportation for HCBS provided through a 1915(c) waiver program for persons with intellectual disabilities (i.e., mental retardation) and HCBS provided through the CHOICES program, except as provided in Section 2.11.1.8.1 above. |
| 67. | Section 2.11.6.3, 2.11.6.4, 2.11.6.6.2, 2.11.6.6.5, 2.11.6.6.7 and 2.11.6.6.8 shall be amended by adding the word “CHOICES” in front of the word HCBS. |
68. Section 2.11.8.4 through 2.11.8.4.2 shall be deleted and replaced as follows:
| 2.11.8.4 | Credentialing of Long-Term Care Providers |
| 2.11.8.4.1 | The CONTRACTOR shall develop and implement a process for credentialing and recredentialing long-term care providers. The CONTRACTOR’s process shall, as applicable, meet the minimum NCQA requirements as specified in the NCQA Standards and Guidelines for the Accreditation of MCOs. In addition, the CONTRACTOR shall ensure that all longterm care providers, including those credentialed/recredentialed in accordance with NCQA Standards and Guidelines for the Accreditation of MCOs, meet applicable State requirements, as specified by TENNCARE in State Rule, this Agreement, or in policies or protocols. |
| 2.11.8.4.1.1 | The CONTRACTOR shall develop policies that specify by HCBS provider type the credentialing process, the recredentialing process including frequency, and ongoing provider monitoring activities. |
| 2.11.8.4.1.1.1 | Ongoing CHOICES HCBS providers must be recredentialed at least annually; |
| 2.11.8.4.1.1.2 | All other CHOICES HCBS providers (e.g., pest control and assistive technology), must be recredentialed, at a minimum, every three (3) years. |
| 2.11.8.4.1.2 | At a minimum, credentialing of LTC providers shall include the collection of required documents, including disclosure statements, and verification that the provider: |
| 2.11.8.4.1.2.1 | Has a valid license or certification for the services it will contract to provide as required pursuant to State law or rule, or TENNCARE policies or protocols; |
| 2.11.8.4.1.2.2 | Is not excluded from participation in the Medicare or Medicaid programs; |
| 2.11.8.4.1.2.3 | Has a National Provider Identifier (NPI) Number, where applicable, and has obtained a Medicaid provider number from TENNCARE. |
| 2.11.8.4.1.2.4 | Has policies and processes in place to conduct, in accordance with Federal and State law and rule and TENNCARE policy, criminal background checks, which shall include a check of the Tennessee Abuse Registry, Tennessee Felony Offender Registry, National and Tennessee Sexual Offender Registry, and List of Excluded Individuals/Entities (LEIE), on all prospective employees who will deliver CHOICES HCBS and to document these in the worker’s employment record; |
| 2.11.8.4.1.2.5 | Has a process in place to provide and document initial and ongoing education to its employees who will provide services to CHOICES members that includes, at a minimum: |
| 2.11.8.4.1.2.5.1 | Caring for Elderly and Disabled population; |
| 2.11.3.4.1.2.5.2 | Abuse and neglect prevention, identification and reporting; |
| 2.11.3.4.1.2.5.3 | Critical incident reporting; |
| 2.11.3.4.1.2.5.4 | Documentation of service delivery; |
| 2.11.3.4.1.2.5.5 | Use of the EVV System; and |
| 2.11.8.4.1.2.5.6 | Any other training requirements specified by TENNCARE in State Rule, this Agreement, or in policies or protocols. |
| 2.11.8.4.1.2.6 | Has policies and processes in place to ensure: |
| 2.11.8.4.1.2.6.1 | Compliance with the CONTRACTOR’s critical incident reporting and management process; and |
| 2.11.8.4.1.2.6.2 | Appropriate use of the EVV system. |
| 2.11.8.4.1.3 | At a minimum, recredentialing of HCBS providers shall include verification of continued licensure and/or certification (as applicable), and compliance with policies and procedures identified during credentialing, including background checks and training requirements, critical incident reporting and management, and use of the EVV. |
| 2.11.8.4.1.4 | For both credentialing and recredentialing processes, the CONTRACTOR shall conduct a site visit, unless the provider is located out of state, in which case the CONTRACTOR may waive the site visit and document the reason in the provider file. |
| 2.11.8.4.1.5 | At a minimum, the CONTRACTOR shall reverify monthly that each HCBS provider has not been excluded from participation in the Medicare or Medicaid, and/or SCHIP programs. |
| 69. | Section 2.12.9.38 shall be amended by adding the word “CHOICES” in front of the word |
“HCBS”.
| 70. | Section 2.12.9 shall be amended by adding a new Section 2.12.9.63 as follows: |
| 2.12.9.63 | The provider, subcontractor or any other entity agrees to abide by the Medicaid laws, regulations and program instructions that apply to the provider. The provider, subcontractor or any other entity understands that payment of a claim by TennCare or a TennCare Managed Care Contractor and/or Organization is conditioned upon the claim and the underlying transaction complying with such laws, regulations, and program instructions (including, but not limited to, the Federal anti-kickback statute and the Xxxxx law), and is conditioned on the provider’s , subcontractor’s or any other entity’s compliance with all applicable conditions of participation in Medicaid. The provider, subcontractor or any other entity understands and agrees that each claim the provider, subcontractor or any other entity submits to TennCare or a TennCare Managed Care Contractor and/or Organization constitutes a certification that the provider, subcontractor or any other entity has complied with all applicable Medicaid laws, regulations and program instructions (including, but not limited to, the Federal anti-kickback statute and the Xxxxx law), in connection with such claims and the services provided therein. |
| 71. | Sections 2.12.12 through 2.12.12.10 and Section 2.12.13 shall be deleted and replaced as follows: |
| 2.12.12 | The provider agreement with a CHOICES HCBS provider shall meet the minimum requirements specified in Section 2.12.9 above and shall also include, at a minimum, the following requirements: |
| 2.12.12.1 | Require the CHOICES HCBS provider to provide at least thirty (30) days advance notice to the CONTRACTOR when the provider is no longer willing or able to provide services to a member, including the reason for the decision, and to cooperate with the member’s care coordinator to facilitate a seamless transition to alternate providers; |
| 2.12.12.2 | In the event that a CHOICES HCBS provider change is initiated for a member, require that, regardless of any other provision in the provider agreement, the transferring HCBS provider continue to provide services to the member in accordance with the member’s plan of care until the member has been transitioned to a new provider, as determined by the CONTRACTOR, or as otherwise directed by the CONTRACTOR, which may exceed thirty (30) days from the date of notice to the CONTRACTOR; |
| 2.12.12.3 | Specify that reimbursement of a CHOICES HCBS provider shall be contingent upon the provision of services to an eligible member in accordance with applicable federal and state requirements and the member’s plan of care as authorized by the CONTRACTOR, and must be supported by detailed documentation of service delivery to support the amount of services billed, including at a minimum, the date, time and location of service, the specific HCBS provided, the name of the member receiving the service, the name of the staff person who delivered the service, the detailed tasks and functions performed as a component of each service, notes for other caregivers (whether paid or unpaid) regarding the member or his/her needs (as applicable), and the initials or signature of the staff person who delivered the service; |
| 2.12.12.4 | Require CHOICES HCBS providers to immediately report any deviations from a member’s service schedule to the member’s care coordinator; |
| 2.12.12.5 | Require CHOICES HCBS providers to use the electronic visit verification system specified by the CONTRACTOR in accordance with the CONTRACTOR’s requirements; |
| 2.12.12.6 | Require that upon acceptance by the CHOICES HCBS provider to provide approved services to a member as indicated in the member’s plan of care, the provider shall ensure that it has staff sufficient to provide the service(s) authorized by the CONTRACTOR in accordance with the member’s plan of care, including the amount, frequency, duration and scope of each service in accordance with the member’s service schedule; |
| 2.12.12.7 | Require CHOICES HCBS providers to provide back-up for their own staff if they are unable to fulfill their assignment for any reason and ensure that back-up staff meet the qualifications for the authorized service; |
| 2.12.12.8 | Prohibit CHOICES HCBS providers from requiring a member to choose the provider as provider of multiple services as a condition of providing any service to the member; |
| 2.12.12.9 | Prohibit CHOICES HCBS providers from soliciting members to receive services from the provider including: |
| 2.12.12.9.1 | Referring an individual for CHOICES screening and intake with the expectation that,, should CHOICES enrollment occur, the provider will be selected by the member as the service provider; or |
| 2.12.12.9.2 | Communicating with existing CHOICES members via telephone, face-to-face or written communication for the purpose of petitioning the member to change CHOICES providers; |
| 2.12.12.10 | Require CHOICES HCBS providers to comply with critical incident reporting and management requirements (see Section 2.15.7 of this Agreement); and |
| 2.12.12.11 | Shall not require the CHOICES HCBS provider to have liability insurance in excess of TENNCARE requirements in effect prior to the implementation of CHOICES. |
| 2.12.13 | The provider agreement with a CHOICES HCBS provider to provide PERS, assistive technology, minor home modifications, or pest control shall meet the requirements specified in Sections 2.12.9, 2.12.10, and 2.12.12 except that these provider agreements shall not be required to meet the following requirements: Section 2.12.9.9 regarding emergency services; Section 2.12.9.11 regarding delay in prenatal care; Section 2.12.9.12 regarding CLIA; Section 2.12.9.38 regarding hospital protocols; Section 2.12.9.40 regarding reimbursement of obstetric care; Section 2.12.9.52.2 regarding prior authorization of pharmacy; and Section 2.12.9.53 regarding coordination with the PBM. |
| 72. | Sections 2.13.3 through 2.13.3.3 and Sections 2.13.4 through 2.13.4.4 shall be deleted and replaced as follows: |
| 2.13.3 | Nursing Facility Services |
| 2.13.3.1 | The CONTRACTOR shall reimburse contract nursing facility providers at the per diem rate specified by TENNCARE, net of any applicable patient liability amount (see Section 2.6.7). |
| 2.13.3.2 | The CONTRACTOR shall reimburse non-contract nursing facility providers as specified in TennCare rules and regulations, net of any applicable patient liability amount (see Section 2.6.7). |
| 2.13.3.3 | If, prior to the end date specified by TENNCARE in its approval of Level II nursing facility services, the CONTRACTOR determines that the nursing facility is providing Level I and not Level II nursing facility services, the CONTRACTOR shall notify TENNCARE and, as appropriate, shall submit a request to modify the member’s level of nursing facility services. The CONTRACTOR shall submit documentation as specified by TENNCARE to support the request. The CONTRACTOR may reimburse the nursing facility for the lesser level of services only when such lesser level of services is billed by the nursing facility or upon approval from TENNCARE of a reduction in the member’s level of care or reimbursement as reflected on the outbound 834 enrollment file. |
| 2.13.3.4 | The CONTRACTOR shall, upon receipt of notification from TENNCARE of a retrospective adjustment of a nursing facility’s per diem rate(s), without requiring any action on the part of the provider, reprocess affected claims and provide any additional payment due within sixty (60) days of receipt of such notification. The CONTRACTOR shall, upon notification in the outbound 834 enrollment file of retroactive patient liability amounts or retroactive adjustments in patient liability amounts, without requiring any action on the part of the provider, reprocess affected claims and provide any additional payment due within thirty (30) days of receipt of such notification. The CONTRACTOR shall not require that NFs resubmit affected claims in order to process these adjustments. |
| 2.13.4 | CHOICES HCBS |
| 2.13.4.1 | For covered CHOICES HCBS and for CHOICES HCBS that exceed the specified benefit limit and are provided by the CONTRACTOR as a cost effective alternative (see Section 2.6.5), the CONTRACTOR shall reimburse contract HCBS providers, including community- based residential alternatives, at the rate specified by TENNCARE. |
| 2.13.4.2 | The CONTRACTOR shall reimburse non-contract CHOICES HCBS providers as specified in TennCare rules and regulations. |
| 2.13.4.3 | For other HCBS that are not otherwise covered but are offered by the CONTRACTOR as a cost effective alternative to nursing facility services (see Section 2.6.5), the CONTRACTOR shall negotiate the rate of reimbursement. |
| 2.13.4.4 | The CONTRACTOR shall reimburse consumer-directed workers in accordance with Sections 2.9.6.7 and 2.26 of this Agreement. |
| 73. | Section 2.13 shall be amended by adding a new Section 2.13.8 as follows and renumbering the existing Section 2.13.8 through 2.13.20 accordingly, including any references thereto. |
2.13.8 Federally Qualified Health Centers and Rural Health Clinics (FQHCs/RHCs)
Upon notification by TENNCARE, the CONTRACTOR shall reimburse contracted FQHCs/RHCs using prospective payment system rates and wraparound payments for qualifying visits in accordance with TENNCARE developed policies and protocols. TENNCARE’s policies and protocols shall be based on federal regulations.
| 74. | The renumbered Sections 2.13.11.3 and 2.13.12.3 shall be amended by adding the words “outbound 834” in front of the words “enrollment file”. |
| 75. | The renumbered Section 2.13.13 shall be amended by adding the phrase “in accordance with the requirements of this agreement” to the end of the last sentence. |
| 2.13.13 | Medically Necessary Services Obtained from Non-Contract Provider Referred by Contract Provider |
The CONTRACTOR shall pay for any medically necessary covered services provided to a member by a non-contract provider at the request of a contract provider. The CONTRACTOR’s payment shall not be less than eighty percent (80%) of the rate that would have been paid by the CONTRACTOR if the member had received the services from a contract provider. The CONTRACTOR shall only pay for covered long-term care services for which the member was eligible (see Section 2.6) and that were authorized by the CONTRACTOR in accordance with the requirements of this agreement.
| 76. | The renumbered Section 2.13.21 shall be amended by adding the phrase “eligible CHOICES” in front of the word “HCBS”. |
| 77. | Section 2.14.1.12 through 2.14.1.12.2 shall be deleted and replaced as follows: |
| 2.14.1.12 | Nursing Facility |
| 2.14.1.12.1 | The CONTRACTOR shall ensure that reimbursement of level II nursing facility care is provided for CHOICES members who have been determined by TENNCARE to be eligible for Level II nursing facility care for the period specified by TENNCARE, except when a lesser level of services is billed by the nursing facility. The CONTRACTOR shall monitor the member’s condition, and if the CONTRACTOR determines that, prior to the end date specified by TENNCARE, the member no longer requires Level II nursing facility care, the CONTRACTOR may submit to TENNCARE a request to modify the member’s level of nursing facility services. The CONTRACTOR shall submit documentation as specified by TENNCARE to support the request. The CONTRACTOR may reimburse the nursing facility for the lesser level of services only when such lesser level of services is billed by the nursing facility or upon approval from TENNCARE of a reduction in the member’s level of care or reimbursement as reflected on the outbound 834 enrollment file. . |
| 78. | Section 2.14.5 through 2.14.5.4 shall be deleted and replaced as follows: |
| 2.14.5 | Authorization of Long-Term Care Services |
| 2.14.5.1 | The CONTRACTOR shall have in place an authorization process for covered long-term care services and cost effective alternative services that is separate from but integrated with the CONTRACTOR’s prior authorization process for covered physical health and behavioral health services (See section 2.9.6 of this Agreement). |
| 2.14.5.2 | The CONTRACTOR may decide whether it will issue service authorizations for nursing facility services, or whether it will instead process claims for such services in accordance with the level of care and/or reimbursement (including the duration of such level of care and/or reimbursement) approved by TENNCARE (see Section 2.14.1.12), except that the CONTRACTOR may reimburse a lesser level of service when such lesser level of service is billed by the facility. |
| 2.14.5.3 | The CONTRACTOR shall authorize and initiate CHOICES HCBS for CHOICES members within the timeframes specified in Sections 2.9.2, 2.9.3, and 2.9.6 of this Agreement. |
| 2.14.5.4 | The CONTRACTOR shall not require that CHOICES HCBS be ordered by a treating physician, but may consult with the treating physician as appropriate regarding the member’s physical health, behavioral health, and long-term care needs and in order to facilitate communication and coordination regarding the member’s physical health, behavioral health, and long-term care services. |
| 2.14.5.5 | For non-CHOICES members receiving care in non-contract nursing facilities authorized by the CONTRACTOR as a cost-effective alternative, the CONTRACTOR shall reimburse services in accordance with its authorization until such time that the member is no longer eligible for services, is enrolled in CHOICES, or such care is no longer medically necessary or cost-effective. |
| 79. | Section 2.14.8.1 shall be deleted and replaced as follows: |
| 2.14.8.1 | The CONTRACTOR is responsible for eliciting pertinent medical history information from the treating provider(s), as needed, for purposes of making medical necessity determinations. With respect to CHOICES HCBS which are not primarily medical in nature, pertinent medical history shall include assessments, case notes, and documentation of service delivery by HCBS providers. Medical information from the treating physician may also be pertinent in better understanding the member’s functional needs. The CONTRACTOR shall take action (e.g., sending a CONTRACTOR representative to obtain the information and/or discuss the issue with the provider, imposing financial penalties against the provider, etc.), to address the problem if a treating provider is uncooperative in supplying needed information. The CONTRACTOR shall make documentation of such action available to TENNCARE, upon request. Providers who do not provide requested information for purposes of making a medical necessity determination for a particular item or service shall not be entitled to payment for the provision of such item or service. |
| 80. | Section 2.15.1.6 shall be amended by adding new Sections 2.15.1.6.1 through 2.15.1.6.3 as follows. |
| 2.15.1.6 | The CONTRACTOR shall take appropriate action to address service delivery, provider, and other QM/QI issues as they are identified. |
| 2.15.1.6.1 | The CONTRACTOR may be required to conduct special focus studies as requested by TENNCARE. |
| 2.15.1.6.2 | The CONTRACTOR shall collect data on race and ethnicity. As part of the QM/QI program description, the CONTRACTOR shall include the methodology utilized for collecting the data, as well as any interventions taken to enhance the accuracy of the data collected. |
| 2.15.1.6.3 | The CONTRACTOR shall include QM/QI activities to improve healthcare disparities identified through data collection. |
| 81. | Section 2.15.4 shall be deleted and replaced as follows: |
2.15.4 Clinical Practice Guidelines
The CONTRACTOR shall utilize evidence-based clinical practice guidelines in its disease management programs. The guidelines shall be reviewed and revised whenever the guidelines change and at least every two (2) years.
| 82. | Section 2.15.6 shall be amended by adding a new Section 2.15.6.3 as follows: |
| 2.15.6.3 | The CONTRACTOR shall submit annually the Relative Resource Use (RRU) data to TENNCARE within ten (10) business days of receipt from NCQA. The CONTRACTOR shall submit both the Regional and National RRU results. |
| 83. | Sections 2.15.7 through 2.15.7.6 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 84. | Section 2.17.2 shall be amended by adding a new Section 2.17.2.10 as follows: |
| 2.17.2.10 | All educational materials (brochures, scripts etc.) shall be reviewed and updated concurrently with the update of the Clinical Practice Guidelines to assure the materials reflect current evidence-based information. |
| 85. | Section 2.17.4.6, 2.17.4.7.15 and 2.17.7.3.22 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 86. | Section 2.17.7.3.2, 2.17.7.3.10, 2.17.7.3.15, 2.17.7.3.16, 2.17.7.3.18, 2.17.7.3.19 and 2.17.8.6 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 87. | Section 2.18.4.6 shall be deleted and replaced as follows: |
| 2.18.4.6 | The provider service line shall be adequately staffed with staff trained to accurately respond to questions regarding the TennCare program and the CONTRACTOR’s MCO, including but not limited to, covered services, the CHOICES program, TENNderCare, prior authorization and referral requirements, care coordination, and the CONTRACTOR’s provider network. For a period of at least twelve (12) months following the implementation of CHOICES in the Grand Region covered by this Agreement, the CONTRACTOR shall maintain a dedicated queue to assist long-term care providers with enrollment, service authorization, or reimbursement questions or issues and shall ensure that long-term care providers are appropriately notified regarding how to access the dedicated queue for assistance. Such period may be extended as determined necessary by TENNCARE. |
| 88. | Section 2.18.5.3.3 shall be deleted and replaced as follows: |
| 2.18.5.3.3 | Description of the CHOICES program including but not limited to who qualifies for CHOICES (including the three CHOICES groups and enrollment targets for CHOICES Groups 2 and 3); how to enroll in CHOICES; long-term care services available to each CHOICES Group (including benefit limits, cost neutrality cap for members in Group 2, and the expenditure cap for members in Group 3); consumer direction of eligible CHOICES HCBS; self-direction of health care tasks; the level of care assessment and reassessment process; the needs assessment and reassessment processes; requirement to provide services in accordance with an approved plan of care including the amount, frequency, duration and scope of each service in accordance with the member’s service schedule; service authorization requirements and processes; the role of the care coordinator; the role and responsibilities of long-term care and other providers; requirements regarding the electronic visit verification system and the provider’s responsibility in monitoring and immediately addressing service gaps, including back-up staff; how to submit clean claims; and documentation requirements for CHOICES HCBS providers; |
| 89. | Section 2.18.5.3.13 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 90. | Section 2.18.5.3 shall be amended by adding a new Section 2.18.5.3.14 and renumbering the existing Section accordingly, including any references thereto. |
| 2.18.5.3.14 | Information for CHOICES HCBS providers regarding prohibition of facilitating CHOICES referrals with the expectation of being selected as the service provider or petitioning existing CHOICES members to change CHOICES providers. |
| 91. | Section 2.18.6.3.16 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 92. | Section 2.18.6 shall be amended by adding a new Section 2.18.6.5 and renumbering the existing Section accordingly, including any references thereto. |
| 2.18.6.5 | The CONTRACTOR shall develop and implement a training plan to educate long-term care providers regarding compliance with ICD- 10 requirements; |
| 93. | The renumbered Sections 2.18.6.7 and 2.18.6.8 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 2.18.6.7 | For a period of at least twelve (12) months following the implementation of CHOICES in the Grand Region covered by this Agreement, the CONTRACTOR shall conduct monthly education and training for CHOICES HCBS providers regarding the use of the EVV system. Such period may be extended as determined necessary by TENNCARE. |
| 2.18.6.8 | The CONTRACTOR shall provide education and training on documentation requirements for CHOICES HCBS. |
94. Section 2.21.5 through 2.21.5.2 shall be deleted and replaced as follows:
2.2 1.5 Patient Liability
| 2.2 | 1.5.1 TENNCARE will notify the CONTRACTOR of any applicable patient liability amounts for members via the outbound 834 enrollment file. |
| 2.21.5.2 | The CONTRACTOR shall delegate collection of patient liability to the nursing facility or community-based residential alternative facility and shall pay the facility net of the applicable patient liability amount. For members in CHOICES Groups 2 or 3 receiving non-residential CHOICES HCBS, the CONTRACTOR shall collect applicable patient liability amounts. |
| 2.2 | 1.5.3 When TENNCARE notifies the CONTRACTOR of patient liability amounts for CHOICES members via the outbound 834 enrollment file at any time other than the beginning of the month, then the CONTRACTOR shall determine and apply the prorated portion of patient liability for that month. |
| 95. | Section 2.22.4.4 through 2.22.4.4.2 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 96. | Section 2.22.6.3 and 2.22.6.4.13 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 97. | Section 2.22.6.4.5 shall be deleted and replaced as follows: |
| 2.22.6.4.5 | Allowed payment amount agrees with contracted rate and the terms of the provider agreement; |
| 98. | Section 2.22.7.1.8 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 99. | Section 2.23.5.1 shall be amended by adding the words “outbound 834” in front of the words “enrollment files”. |
| 100. | Section 2.23.13.1 shall be amended by adding the words “outbound 834” in front of the words “enrollment file”. |
| 101. | Section 2.24.3.2 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 102. | Section 2.26.6 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS. |
| 103. | Section 2.29.1 shall be amended by adding a new Section 2.29.1.11 as follows: |
| 2.29.1.11 | The CONTRACTOR shall be required to have appropriate staff member(s) attend certain on-site meetings held at TennCare offices or at other sites as requested and designated by TENNCARE. |
| 104. | Sections 2.29.2 through 2.29.2.2 shall be deleted and replaced as follows: |
2.29.2 Licensure and Background Checks
| 2.29.2.1 | Except as specified in this Section 2.29.2.1 regarding the FEA, the CONTRACTOR is responsible for ensuring that all persons, whether they are employees, agents, subcontractors, providers or anyone acting for or on behalf of the CONTRACTOR, are legally authorized to render services under applicable state law. The FEA shall be responsible for ensuring that consumer-directed workers are qualified to provide eligible CHOICES HCBS in accordance with TENNCARE requirements. |
| 2.29.2.2 | Except as specified in this Section 2.29.2.2 regarding the FEA, the CONTRACTOR is responsible for conducting background checks in accordance with state law and TennCare policy and ensuring that all employees, agents, subcontractors, providers or anyone acting for or on behalf of the CONTRACTOR conducts background checks in accordance with state law and TennCare policy. At a minimum, background checks shall include a check of the Tennessee Abuse Registry, Tennessee Felony Offender Registry, National and Tennessee Sexual Offender Registry, and List of Excluded Individuals/Entities (LEIE). The FEA shall be responsible for conducting background checks on its staff, its subcontractors, and consumer-directed workers. |
| 105. | Section 2.30.1.4 shall be deleted and replaced as follows: |
| 2.30.1.4 | The CONTRACTOR shall submit all reports electronically and in the manner and format prescribed by TENNCARE and shall ensure that all reports are complete and accurate. The CONTRACTOR shall be subject to liquidated damages as specified in Section 4.20.2.1.1 for reports determined to be late, incorrect, incomplete or deficient, or not submitted in the manner and format prescribed by TENNCARE until all deficiencies have been corrected. Except as otherwise specified by TENNCARE, all reports shall be specific to the Grand Region covered by this Agreement. |
| 106. | The lead in paragraph of Section 2.30.6.5 shall be deleted and replaced as follows: |
| 2.30.6.5 | The CONTRACTOR shall submit a monthly CHOICES HCBS Late and Missed Visits Report for CHOICES members regarding the following CHOICES HCBS: personal care, attendant care, homemaker services, and home-delivered meals. The report shall include information on specified measures, which shall include but not be limited to the following: |
| 107. | Item (2) of Section 2.30.6.6 shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 108. | Section 2.30.7.1 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 109. | Section 2.30.7.5 shall be deleted and replaced as follows: |
| 2.30.7.5 | The CONTRACTOR shall submit an Annual Plan for the Monitoring of Behavioral Health Appointment Timeliness that shall include the CONTRACTOR’s plan for monitoring behavioral health providers to ensure that they comply with the timeliness of appointment standards that are outlined for behavioral health in Attachment III for routine specialty MD (behavioral health) care and Attachment V for Outpatient Non-MD behavioral health services. This plan will be submitted for approval to the Bureau of TennCare by December 31 of each year and shall identify methods for determining how they will monitor and evaluate providers for compliance, develop corrective action plans for compliance, maintain records of audits for timeliness and describe efforts to improve timeliness of appointments. The minimum data elements required are identified in Attachment IX, Exhibit D. |
| 110. | Section 2.30.7 shall be amended by adding a new Section 2.30.7.6 and renumbering the existing Sections 2.30.7.6 and 2.30.7.7 accordingly, including any references thereto. |
| 2.30.7.6 | The CONTRACTOR shall submit a Quarterly Behavioral Health Appointment Timeliness Summary Report that includes a quarterly summary of activities based on the Annual Plan for Monitoring of Behavioral Health Appointment Timeliness (See Section 2.30.7.5) The minimum data elements required are identified in Attachment IX, Exhibit D. |
| 111. | Section 2.30.9 shall be amended by adding a new Section 2.30.9.5 as follows: |
| 2.30.9.5 | Upon notification by TENNCARE, the CONTRACTOR shall submit a weekly Administrative Services Only Invoice Report for all payments to clinics designated as Federally Qualified Health Clinics or Rural Health Clinics. |
| 112. | Section 2.30.11 shall be amended by adding a new Section 2.30.11.7 as follows: |
| 2.30.11.7 | By October 1, 2011, the CONTRACTOR is required to submit a Data Collection Strategy Report that describes how they intend to collect data in accordance with the HHS initiative to implement a multifaceted health disparities data collection strategy. (HHS Action Plan to Reduce Racial and Ethnic Health Disparities, April 8, 2011) The report must include the CONTRACTOR’s plans for collection and reporting of data in five specific demographic categories in accordance with the new provisions of the Affordable Care Act: race, ethnicity, gender, primary language, and disability status. The following OMB (minimum standards) categories for race and ethnicity (Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity, 1997) must be used: Hispanic or Latino or Not Hispanic or Latino; American Indian or Alaska Native, Asian, Black or African American, Hispanic or Latino, Native Hawaiian or Other Pacific Islander, and White. CONTRACTOR plans must also include how the collected data will be used to integrate information across systems in order to enhance TennCare data, any system changes that will be needed, and timelines for implementation. Following review of the CONTRACTOR’s plan, TENNCARE will set an implementation date for revised data collection and data reporting. |
| 113. | Item (2) of Section 2.30.16.4 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 114. | Section 3.1.2 shall be amended by adding the phrase “, any payments related to FQHC/RHC costs” as follows: |
| 3.1.2 | The CONTRACTOR agrees that capitation payments, any payments related to processing claims for services incurred prior to the start date of operations pursuant to Section 3.7.1.2.1, any incentive payments (if applicable), any payments related to FQHC/RHC costs and any payments that offset the CONTRACTOR’s cost for the development and implementation of an electronic visit verification system (EVV) (see Section 3.13) are payment in full for all services provided pursuant to this Agreement. TENNCARE shall not reimburse CONTRACTOR for any costs, liquidated damages and/or penalties incurred by the CONTRACTOR and which result from actions or inactions, including penalties associated with CONTRACTOR’s failure to timely pay any and all expenses, fees, taxes and other regulatory/ministerial costs associated with the requirements of operating as an HMO in this state. The taxes, fees, expenses, and other regulatory/ministerial costs referenced herein shall include but not be limited to premium taxes associated with any and all obligations required by the Tennessee Health Maintenance Organization Act of 1986 codified at TCA 00-00-000 et seq. or any subsequent amendments thereto and/or the Tennessee Prepaid Limited Health Services Act of 2000 codified at TCA 00-00-000 et seq. or any subsequent amendments thereto. TENNCARE shall not share with the CONTRACTOR any financial losses realized under this Agreement. |
| 115. | Section 3.4.3.7.1.1.1 shall be amended as follows: |
| 3.4.3.7.1.1.1 | CHOICES members that change MCOs during the open enrollment period will be designated as either a NF enrollee or an HCBS enrollee based upon the determination made in the outbound 834 enrollment file on the date of their official transfer. |
| 116. | Section 3.7.1 shall be amended by adding a new Section 3.7.1.5 and 3.7.1.6, deleting and replacing the renumbered Section 3.7.1.7 as follows and updating all references accordingly. |
| 3.7.1.5 | The CONTRACTOR shall not be entitled to a CHOICES capitation payment for any calendar month during which a CHOICES member does not receive nursing facility services or ongoing CHOICES HCBS, except under extenuating circumstances which must be reported to TENNCARE on the CHOICES Utilization Report. Acceptable extenuating circumstances may include, but are not limited to, a member’s temporary hospitalization or temporary receipt of Medicare-reimbursed skilled nursing facility care. The determination that the CONTRACTOR is not entitled to a CHOICES capitation payment shall be made by TENNCARE based on information provided in monthly CHOICES Utilization Reports and/or upon review and analysis of the CONTRACTOR’s encounter data. For any month in which the CONTRACTOR is not entitled to the CHOICES capitation payment, the capitation payment will be retroactively adjusted to reflect the appropriate non-CHOICES capitation rate applicable for that month. |
| 3.7.1.6 | The effective date of the CHOICES capitation payment may be retroactively adjusted by TENNCARE in any instance in which the CONTRACTOR fails to initiate nursing facility services or ongoing CHOICES HCBS within the timeframes prescribed in 2.9.6., in which case, the effective date of the CHOICES capitation payment will be the date of initiation of nursing facility or ongoing HCBS. |
| 3.7.1.7 | Payment adjustments resulting in a reduction or increase of the capitation rate shall be accomplished through the monthly capitation reconciliation process, or pursuant to other processes as established by TENNCARE. |
| 117. | Section 3.9.2.6 shall be deleted and replaced as follows: |
| 3.9.2.6 | The withhold amounts for subsequent months thereafter in which the CONTRACTOR has not cured the deficiencies shall be in accordance with Section 3.9.2.1 as described above. If the CONTRACTOR has attained a two and one half percent (2.5%) withhold and TENNCARE subsequently determines the CONTRACTOR is not in compliance with a requirement of this Agreement, TENNCARE will provide written notice of such determination and TENNCARE will re-institute the retention of the withhold as described in Section 3.9.2.1 at the next capitation payment cycle. Monthly retention of the withhold amount will continue for each subsequent month so long as the identified deficiencies have not been corrected. These funds will not be distributed to the CONTRACTOR unless it is determined by TENNCARE the CONTRACTOR has come into compliance with the Agreement requirement(s) within six (6) months of TENNCARE identifying these deficiencies. For example, if a specified deficiency(s) is corrected within four (4) months and there are no other identified deficiencies which the CONTRACTOR has been given written notice of by TENNCARE, the withhold for the four (4) consecutive months will be paid to the CONTRACTOR upon TENNCARE determination that the deficiency(s) was corrected. However, any amounts withheld by TENNCARE for six (6) consecutive months for the same or similar compliance deficiency(s) shall be permanently retained by TENNCARE on the first day after the sixth consecutive month period and shall not be paid to the CONTRACTOR. If the same or similar specified deficiency(s) continues beyond six (6) consecutive months, TENNCARE may declare the MCO ineligible for future distribution of the ten percent (10%) incentive withhold and may continue to permanently retain any amounts withheld by TENNCARE for six (6) consecutive months. Such ineligibility will continue for each month TENNCARE determines the same or similar specified deficiency(s) continues to exist. Once a CONTRACTOR corrects the deficiency(s), TENNCARE may reinstate the MCO’s eligibility for distribution of the ten percent (10%) compliance incentive payment of future withholds. If TENNCARE determines that distribution of the ten percent (10%) withhold is appropriate, distribution of the ten percent (10%) shall be made at the time of the next scheduled monthly check write which includes all other payments due the CONTRACTOR. |
| 118. | Section 3 shall be amended by adding a new Section 3.11 as follows and renumbering the existing Sections 3.11 through 3.14 accordingly including any references thereto. |
3.11 Reimbursement of Cost related Payments for FQHCs/RHCs
Upon notification by TENNCARE, TENNCARE shall reimburse the CONTRACTOR for FQHC/RHC cost outside of the capitation rates in accordance with TENNCARE developed policies and protocols and based on the CONTRACTOR’s reported Administrative Services Only weekly invoice (See Section 2.30.9.5). TENNCARE’s policies and protocols shall be based on federal regulations.
| 119. | The renumbered Section 3.15.1.1 shall be deleted and replaced as follows: |
| 3.15.1.1 | In no event shall the maximum liability of the State under this Agreement during the original term of the Agreement exceed four billion, two hundred thirty million, nine hundred ten thousand,eight hundred sixty nine dollars ($4,230,910,869.00). |
| 120. | The opening paragraph of Section 4.1 shall be deleted and replaced as follows: |
4.1 NOTICE
All notices required to be given under this Agreement shall be given in writing, and shall be sent by United States certified mail, postage prepaid, return receipt requested; in person; by facsimile, email or other electronic means, including but not limited to providing notice through computer databases, software or other systems made available to the CONTRACTOR by TENNCARE; or by other means, so long as proof of delivery and receipt is given, and the cost of delivery is borne by the notifying party, to the appropriate party at the address given below, or at such other address (or addresses) as may be provided by notice given under this Section.
121. Section 4.2.1 and 4.2.2 shall be deleted and replaced as follows: 4.2.1 Term of the Agreement
This Agreement, including any amendments and any changes made by notice to adjust the capitation rates, shall be effective commencing on August 15, 2006 and ending on December 31, 2014.
4.2.2 Term Extension
The State reserves the right to extend this Agreement for an additional period or periods of time representing increments of no more than one (1) year and a total term of no more than five (5) years, provided that the State notifies the CONTRACTOR in writing of its intention to do so at least six (6) months prior to the Agreement expiration date. In accordance with an approved exception request, TENNCARE may extend this Agreement through December 31, 2014. An extension of the term of this Agreement will be effected through an amendment to the Agreement.
| 122. | Section 4.20.2.1.1 shall be amended by adding the word “incomplete” as follows: |
| 4.20.2.1.1 | For each day that a report or deliverable is late, incorrect, incomplete, or deficient, the CONTRACTOR shall be liable to TENNCARE for liquidated damages in the amount of one hundred dollars ($100) per day per report or deliverable unless specified otherwise in this Section. Liquidated damages for late reports/deliverables shall begin on the first day the report/deliverable is late. |
| 123. | The liquidated damage chart in Section 4.20.2.2.7 shall be amended by deleting and replacing A.20 and adding new damages A.21 through A.26 as follows: |


 |
| 124. | Section C of the Program Issues/Damages chart of Section 4.20.2.2.7 shall be amended by adding a new C.3 as follows and renumbering the existing C.3 through C.7 as follows including any references thereto. |

| 125. | Section 4.20.2.4 shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 126. | Section 4 shall be amended by adding new Sections 4.38 and 4.39 as follows and the existing Sections 4.38 and 4.39 shall be renumbered accordingly including any references thereto. |
4.38 Prohibition of Payments for Items or Services Outside the United States
Section 6505 of the Affordable Care Act amends section 1902(a) of the Social Security Act (the Act), and requires that a State shall not provide any payments for items or services provided under the State plan or under a waiver to any financial institution or entity located outside of the United States (U.S.). This section of the Affordable Care Act is effective January 1, 2011, unless the Secretary determines that implementation requires State legislation, other than legislation appropriating funds, in order for the plan to comply with this provision.
For purposes of implementing this provision, section 110 1(a)(2) of the Act defines the term “United States” when used in a geographical sense, to mean the “States.” Section 1 101(a)(1) of the Act defines the term “State” to include the District of Columbia, Puerto Rico, the Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa, when used under Title XIX.
Further, this provision prohibits payments to telemedicine providers located outside of the U.S., Puerto Rico, the Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa. Additionally, payments to pharmacies located outside of the U.S., Puerto Rico, the Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa are not permitted.
The Centers for Medicare & Medicaid Services (CMS) will require that, in the case of providers that have provided medical assistance or covered items and/or services to Medicaid beneficiaries under the State plan or under a waiver program, and are requesting reimbursement from the State Medicaid program, such reimbursement must be provided to financial institutions or entities located within the U.S. If it is found that payments have been made to financial institutions or entities outside of the U.S., States must recover these payments and must forward any Federal match for such payments to CMS consistent with the guidelines specified in Federal regulations at 42 CFR Part 433.
Any audits of claims by CMS to assure compliance with this provision will begin no earlier than June 1, 2011 and will only review claims submitted on or after June 1, 2011 for compliance with this section.
4.39 Federal Funding Accountability and Transparency Act (FFATA)
This Agreement requires the CONTRACTOR to provide supplies and/or services that are funded in whole or in part by federal funds that are subject to FFATA. The CONTRACTOR is responsible for ensuring that all applicable requirements, including but not limited to those set forth herein, of FFATA are met and that the CONTRACTOR provides information to the State as required.
The CONTRACTOR shall comply with the following:
| 4.39.1 | Reporting of Total Compensation of the CONTRACTOR’s Executives. |
| 4.39.1.1 | The CONTRACTOR shall report the names and total compensation of each of its five most highly compensated executives for the CONTRACTOR’s preceding completed fiscal year, if in the CONTRACTOR’s preceding fiscal year it received: |
| 4.39.1.1.1 | Eighty percent (80%) or more of the CONTRACTOR’s annual gross revenues from Federal procurement contracts and Federal financial assistance subject to the Transparency Act, as defined at 2 CFR 170.3 20 (and sub awards); and |
| 4.39.1.1.2 | $25,000,000 or more in annual gross revenues from Federal procurement contracts (and subcontracts), and Federal financial assistance subject to the Transparency Act (and sub awards); and |
| 4.39.1.1.3 | The public does not have access to information about the compensation of the executives through periodic reports filed under section 13(a) or 15(d) of the Securities Exchange Act of 1934 (15 U.S.C. 78m(a), 78o(d)) or section 6104 of the Internal Revenue Code of 1986. (To determine if the public has access to the compensation information, see the U.S. Security and Exchange Commission total compensation filings at xxxx://xxx.xxx.xxx/xxxxxxx/xxxxxxx.xxx.). |
Executive means officers, managing partners, or any other employees in management positions.
| 4.39.1.2 | Total compensation means the cash and noncash dollar value earned by the executive during the CONTRACTOR’s preceding fiscal year and includes the following (for more information see 17 CFR 229.402(c)(2)): |
| 4.39.1.2.1 | Salary and bonus. |
| 4.39.1.2.2 | Awards of stock, stock options, and stock appreciation rights. Use the dollar amount recognized for financial statement reporting purposes with respect to the fiscal year in accordance with the Statement of Financial Accounting Standards No. 123 (Revised 2004) (FAS 123R), Shared Based Payments. |
| 4.39.1.2.3 | Earnings for services under non-equity incentive plans. This does not include group life, health, hospitalization or medical reimbursement plans that do not discriminate in favor of executives, and are available generally to all salaried employees. |
| 4.39.1.2.4 | Change in pension value. This is the change in present value of defined benefit and actuarial pension plans. |
| 4.39.1.2.5 | Above-market earnings on deferred compensation which is not tax qualified. |
| 4.39.1.2.6 | Other compensation, if the aggregate value of all such other compensation (e.g. severance, termination payments, value of life insurance paid on behalf of the employee, perquisites or property) for the executive exceeds $10,000. |
| 4.39.2 | The CONTRACTOR must report executive total compensation described above to the State by the end of the month during which this Contract is awarded. |
| 4.39.3 | If this Agreement is amended to extend its term, the CONTRACTOR must submit an executive total compensation report to the State by the end of the month in which the amendment to this Agreement becomes effective. |
| 4.39.4 | The CONTRACTOR will obtain a Data Universal Numbering System (DUNS) number and maintain its DUNS number for the term of this Agreement. More information about obtaining a DUNS Number can be found at: xxxx://xxxxxx.xxx.xxx/xxxxxxx/ |
| 4.39.5 | The CONTRACTOR’s failure to comply with the above requirements is a material breach of this Agreement for which the State may terminate this Agreement for cause. The State will not be obligated to pay any outstanding invoice received from the CONTRACTOR unless and until the CONTRACTOR is in full compliance with the above requirements. |
| 127. | “Timely Claims Processing”, “Claims Payment Accuracy”, and “HCBS Provider Network” Performance Measures in Attachment VII shall be amended by adding the word “CHOICES” in front of the word “HCBS”. |
| 128. | The Performance Measure regarding “Initial appointment timeliness for behavioral health services” in Attachment XII shall be deleted in its entirety. |
| 129. | Item 17 and 120 in Attachment VIII shall be amended by adding the words “eligible CHOICES” in front of the word “HCBS”. |
| 130. | Attachment VIII shall be amended by deleting and replacing Items 129, 131, and 132; adding new Items 130 and 138 as follows and renumbering the existing items accordingly. |
| 129. | Annual Plan for the Monitoring of Behavioral Health Appointment Timeliness (see Section 2.30.7.5) |
130. Quarterly Behavioral Health Appointment Timeliness Summary Report (see Section 2.30.7.6)
131. CHOICES Qualified Workforce Strategies Report (see Section 2.30.7.7)
132. FQHC Reports (see Section 2.30.7.8)
138. Administrative Services Only Invoice Report (See Section 2.30.9.5)
131. Exhibit D of Attachment IX shall be deleted and replaced as follows:
ATTACHMENT IX, EXHIBIT D
Annual Plan and Quarterly Summary for the Monitoring of Behavioral Health Appointment Timeliness
I. Annual Plan for the Monitoring of Behavioral Health Appointment Timeliness
The Annual Plan for the Monitoring of Behavioral Health Appointment Timeliness required in Section 2.30.7.5 will be submitted to the Bureau of TennCare by December 31 of each year, with the first annual plan due for submission by December 31, 2011. This deliverable shall include, at a minimum, the following elements:
| 1. | A plan for how the CONTRACTOR monitors and evaluates behavioral health providers for compliance with the timeliness of appointment standards that are outlined for behavioral health in Attachment III for routine MD (behavioral health) specialty care and Attachment V for Outpatient Non-MD behavioral health services. |
2. The plan shall include a delineation of methodologies used for monitoring and evaluation:
| a. | The plan shall include at minimum, at least one method that incorporates either a phone survey or on- site audit. |
| b. | The report shall include the frequency of surveys/audits, number of site visits, and types of providers monitored, by (MD and non-MD), and by age group (under 18 years of age and 18 years of age and over) as well as number of phone calls or number of appointments evaluated for timeliness, by type (MD/non-MD) and (under 18 years of age and 18 years of age and over) for each provider. |
| 3. | This report will also include the types of correspondence with providers regarding timeliness of appointments; number of performance reports issued to providers, number of Corrective Action Plans (CAPs) issued to providers and results of follow-up to the CAPs. |
| 4. | A summary of overall findings will include a summary of results across providers; how representative the sample of surveys/site visits are of the overall volume of services provided; analysis of data collection and identification and resolution of problems, including percentage of compliance with standards in Attachments III and V, as outlined in # 1 above. |
| 5. | Description of record keeping, including results of audits and surveys, and requests for corrective action plans submitted to providers. |
6. A summary of other methods used to monitor the timeliness of behavioral health appointments.
II. Quarterly Summary for the Monitoring of Behavioral Health Appointment Timeliness
The Quarterly Summary for the Monitoring of Behavioral Health Appointment Timeliness as required in Section 2.30.7.6. will be due within thirty (30) days after completion of the quarter. This deliverable shall include, at a minimum, a summary and update of the quarterly activities and results outlined in the Annual Plan for the Monitoring of Behavioral Health Appointment Timeliness as required in Section 2.30.7.5, including strategies, results and outcomes of efforts to improve timeliness of appointments.
| 132. | Section A.4.3.2.4.1 of Attachment XI shall be amended by deleting “one-quarter (1/4th)” and replacing it with “one-third (1/3)”. |
| A.4.3.2.4.1 The furthest distance a member shall be required to travel to or from a fixed route transportation stop is one-third (1/3) of a mile. |
| 133. | Sections A.12.5 and A.12.6 of Attachment XI shall be deleted and replaced as follows: |
| A.12.5 The CONTRACTOR shall provide Department of Intellectual and Developmental Disabilities (DIDD) residential and day service waiver providers the opportunity to become a NEMT provider if the provider is qualified to provide MR waiver transportation services (either as an individual transportation service or as a component of residential and/or day services) pursuant to provider qualifications applicable for such providers which shall be determined by DIDD. These providers shall only provide covered NEMT services to members receiving HCBS MR waiver services from the provider. The CONTRACTOR shall reimburse these providers for covered NEMT to TennCare covered services (see definition in Exhibit A) and shall not reimburse these providers for NEMT to services provided though a HCBS MR waiver. The CONTRACTOR shall reimburse these providers in accordance with rates paid to other NEMT providers for the provision of NEMT services. |
| A.12.6 The CONTRACTOR shall ensure that its NEMT providers are qualified to perform their duties. Except as specified in A. 12.5, this includes, but is not limited to, meeting applicable federal, state or local licensure, certification, or registration requirements. Failure to comply with requirements regarding licensure requirements may result in liquidated damages as provided in Section 4.20.2 of the Agreement. |
134. Section A.14 of Attachment XI shall be amended by adding a new sentence as follows:
A.14 PAYMENT FOR NEMT SERVICES
A.14.1 General
In addition to requirements in the Agreement regarding payment for services, when paying for NEMT services the CONTRACTOR shall comply with the requirements in this Attachment. In addition to the requirements of this Agreement and this Attachment, the CONTRACTOR shall have a policy to address fuel price adjustments.
135. Item 13 of Exhibit A of Attachment XI shall be deleted and replaced as follows:
| 13. | TennCare Covered Services: The health care services available to TennCare enrollees, as defined in TennCare rules and regulations. This includes, but is not limited to, physical health, behavioral health, pharmacy, dental services, and institutional services. TennCare covered services includes TENNderCare services. For purposes of NEMT, TennCare covered services does not include CHOICES HCBS or 19 15(c) MR waiver services. |
136. Attachment XII shall be amended by adding a new Exhibit E and F as follows:
EXHIBIT E
CAPITATION RATES
AmeriGroup
EFFECTIVE July 1, 2010

EXHIBIT F
CAPITATION RATES
AmeriGroup
EFFECTIVE January 1, 2011
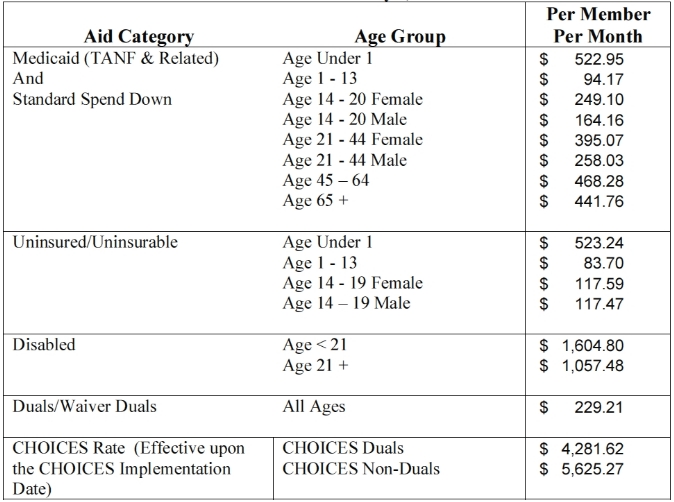
All of the provisions of the original Agreement not specifically deleted or modified herein shall remain in full force and effect. Unless a provision contained in this Amendment specifically indicates a different effective date, for purposes of the provisions contained herein, this Amendment shall become effective July 1, 2011.
IN WITNESS WHEREOF, the parties have by their duly authorized representatives set their signatures.



